Bones made to order: UR Medical Center attempting to use 3-D printing, stem cells to regenerate bone tissue
This news story appeared in the Democrat & Chronicle on February 27, 2017. It features Hani Awad (Biomedical Engineering primary faculty) and Edward Schwarz (Biomedical Engineering graduate faculty), two University of Rochester scientists who are leading the way in using 3-D printers and stem cells to create bone replacements for patients. The online version can be found here.

Imagine getting a made-to-order bone implanted in your body that's composed of your own cells.
Scientists at the University of Rochester Medical Center have been developing a procedure to use 3-D printing and stem cells from the patient to create bones made of regenerated tissue.
This multi-step procedure still has a ways to go before it is tested on humans and can become part of the services provided by URMC's Center for Musculoskeletal Research. But it's the latest example of how 3-D printing, which is increasingly finding its place in manufacturing, is leaving its mark in medicine.
“It is changing the way we do a lot of things,” said Hani Awad, who is associate director of the center and professor of biomedical engineering with a specialty in tissue engineering.
Biomedical research, as it is being done in this initiative, is an important component of the medical center's identity.
"Part of our mission is that we want to do research that is impactful," said Stephen Dewhurst, vice dean for research at the medical center.
Alternative to amputation
UR is already using 3-D printing to create replicas of human organs to practice on before conducting difficult surgical procedures. The Center for Musculoskeletal Research is trying to go beyond this use of 3-D printing.
Edward Schwarz, director of the center, and Awad are heading up an initiative that not only makes replicas of bones for doctors to better understand and show patients the problems they face, but is also using 3-D printing to create the framework for regenerating bone tissue.
Currently, a person with a badly damaged limb that cannot be healed by surgical means faces amputation, followed by the fitting of an artificial limb. Bones from cadavers are also sometimes used as replacement limbs, but there is a high failure rate with cadaver limbs over time. That's because cadaver bones are not living tissue and thus cannot repair themselves when the limb suffers minor fractures, as they often do.
Bone regeneration offers the prospect of a new alternative. The surgically implanted replica serves as a framework to regenerate bone tissue.
"A big part of the problem is figuring out how to grow a big piece of bone," said Awad.
With the technology developed, a 3-D replica is created by taking a CT scan of the patient's bone. What's recorded by the scan is then converted by a computer into a digital model that programs the 3-D printer.
If a leg is too badly damaged to make a replica, a CT scan can be taken of the patient's other leg. And with the use of computer technology, any needed modification can be made. A CT scan of a left leg could be made to look like it is a right leg in the 3-D printout.
During a recent demonstration, the stainless steel platform of the 3-D printer, which moves up and down, was replenished with a supply of powdered calcium phosphate — a material similar to bone. The printer's inkjets were programmed by computer to spray a binding solution of phosphoric acid in a pattern that formed a thighbone. Over the course of an hour or so, the 3-D printer — creating one thin layer on top of another — built the artificial human bone about 1 inch thick and 6 inches long.
But that's not where this bone replacement procedure ends. The next step — and one not yet tried on humans — is regeneration of tissue using stem cells wrapped around the replacement bone. Schwarz and Awad have been testing bone regeneration on mice, without any indication of rejection and with signs of bone regeneration.
And they are beginning to test regeneration on mini-pigs. The 3-D replica bones are coated with sheets of stem cells, which regenerate bone tissue. Eventually, the 3-D part of the replacement bones — made of calcium phosphate — is expected to be absorbed by new bone tissue. Awad estimates that this tissue regeneration technology could be tried on humans in three to five years.
Drawing from strengths
UR is among a handful of universities doing research that combines 3-D technology and tissue regeneration.
"The exact horizon is unclear, but we are certainly running full-speed ahead," said Dr. Paul Rubery, chairman of the Department of Orthopaedics at the UR Medical Center.
3-D printing, Rubery noted, makes possible the reproduction of intricate shapes, including those in the human body.
"What is the science — one might say what is the magic — that will make a person's body take on a new part and make it a living part?" said Rubery about the possibility of bone regeneration using stem cells and 3-D technology.
The Medical Center is well positioned to figure this out.
"We have a long tradition of understanding the molecular processes that lead to healing and repair of the skeleton," said Rubery.
The Musculoskeletal Center, which is in Rubery's department, last fiscal year received the second highest amount of funding for such centers from the National Institutes of Health — roughly $10 million. About 65 researchers and technicians are on staff. The other half of the equation is the Medical Center’s Upstate Stem Cell cGMP Facility, where stem cells are grown in accordance with strict Food and Drug Administration regulations. Located in the Medical Center's Ernest J. Del Monte Neuromedicine Institute, the cGMP was established in 2012, with the help of a $3.5 million grant from the Empire State Stem Cell Board. In bone regeneration, the stem cells are usually taken by syringe at the hip, where such cells are plentiful, and then grown in petri dishes at the cGMP Facility.
Schwarz, who is a professor of orthopaedics, said what's most needed before the procedure can be used on humans is work on how the stem cells are transferred from the cGMP facility to the 3-D replicas.
"You basically have to demonstrate that you can harvest the cells, grow the cells and re-implant the cells in a safe and effective manner," said Schwarz.
Currently, the alternative to an artificial leg is one from a cadaver, but that is done only in limited situations.
"If the bone is not alive, it eventually becomes structurally weakened," said Dewhurst.
Bone grafts are also done, but here, too, the graft comes from cadavers in the vast majority of cases, said Awad.
Regenerating bone tissue would provide a different dynamic — creating live bone tissue that replenishes itself. Rejection is not expected to be an issue because the stem cells would come from the patient. Unlike other cells, stem cells have the capability to divide indefinitely, so they can grow new bone tissue.
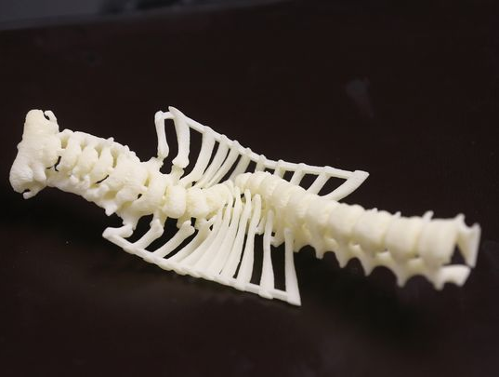
Awad and Schwarz are among the authors of studies in scientific journals that show the effectiveness of stem cells in healing damaged bones in mice. In a laboratory at the Musculoskeletal Center is a tabletop full of replicas of human bones and bone structures made by the 3-D printer in the room. The replica of the spine is that of a child who suffered from a severe curvature. Having such a model enabled a doctor to figure out what kind of steps could be taken to address the problem. The 3-D skull on the table is a replica of a human skull and provides a way researchers can study how injuries can be treated. A hole was made in the cheekbone to resemble a bullet wound. Another replica was missing part of a jaw.
In both cases, the goal is to have stem cells regenerate bone tissue. The body can naturally heal itself in the normal course of injuries, but can't do so when the bone is damaged beyond repair. Implanting a 3-D bone coated with human stem cells would offer an alternative to existing choices.
"It is really going to be part of UR Medicine and its health care system," said Schwarz.
