The Team
Faculty Supervisor: Veena Ganeshan
Liaison: Lucas Lassinger
Customer

Led by Don Gibson, George Reamsnyder, and Tom Kennedy, the student team worked with Curbell Medical.
Background Information & The Problem
Up to a million patients fall in hospitals each year 1. 30% of these falls result in serious injuries that on average cost $27,000 for hospitals 1. 79% of falls in the hospital occur “unassisted”, or without a medical professional present 2. We aim to create a device that uses accelerometers to predict when patients are attempting exit their bed without medical assistance. Our device would benefit patients, their loved ones, medical staff and hospitals.
Current devices often use pressure sensors to determine when a patient has left their bed. These devices are “reactive” and only alert medical staff when the patient has already exited their bed. Our design is more predictive, buying medical staff more time to prevent unassisted movement. It is designed to be worn on the patient’s ankle and chest regions for the duration of their hospital stay.
The Design Process
Electronics
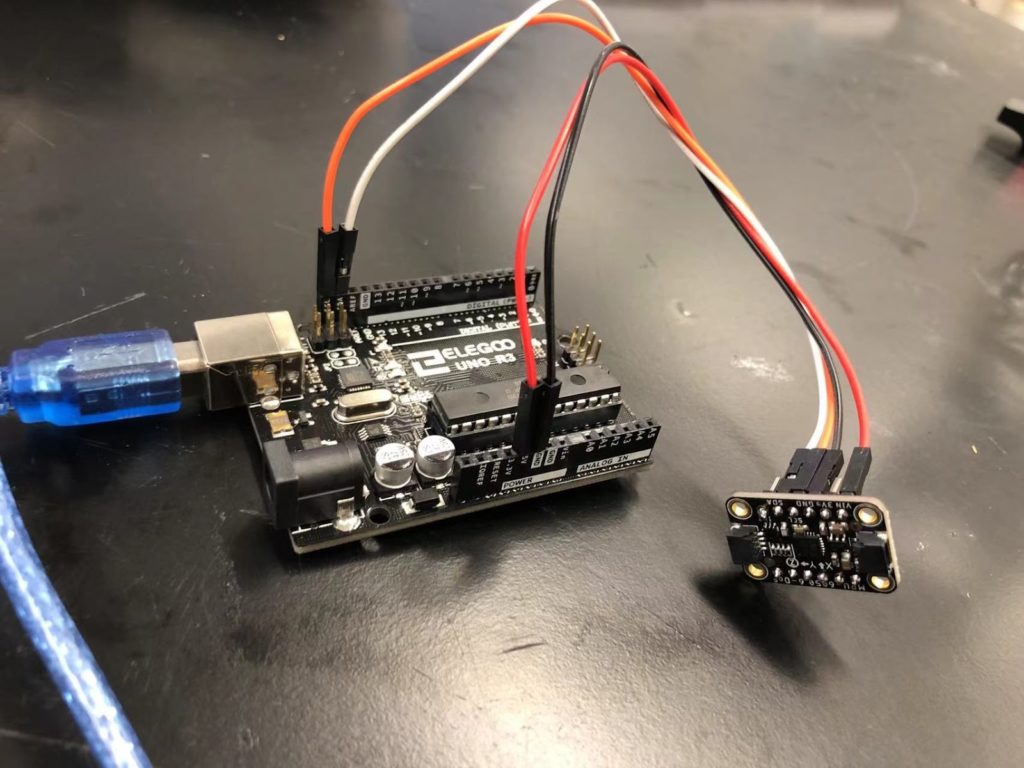
We began with a standard size Arduino board and a 3 axis accelerometer. This worked well but was large and bulky so we made changes to minimize size.
Sensor Pack & Wearable Components
In the beginning, we used some plastic casings that we had on hand in the design lab to make sure the sensors were working. These worked but were bulky and not made to fit our electronics.


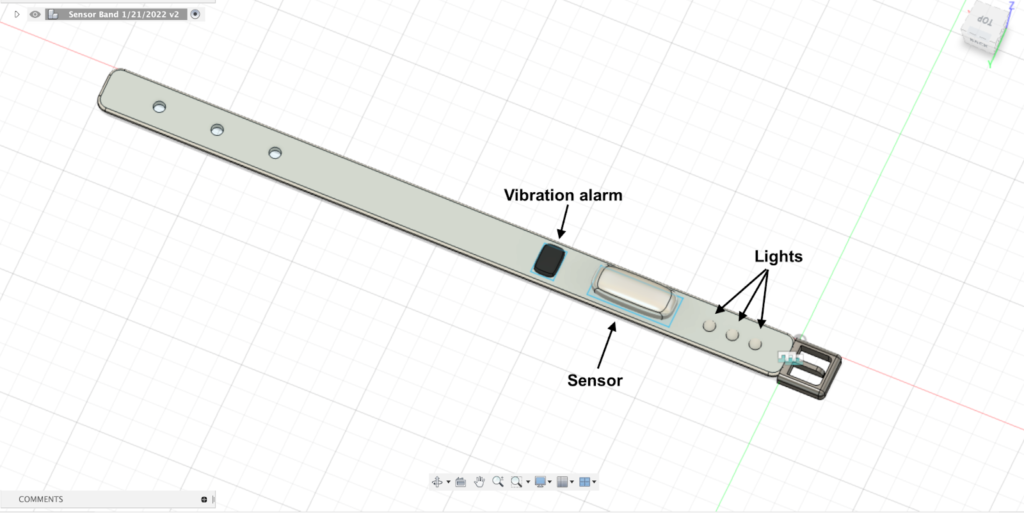
Once we knew the concept worked, we began designing our own sensor packs. Below is a watch-like design. This would be comfortable to wear, but our team probably couldn’t make our electronics small enough. This would also be a more expensive device to manufacture.
We then started working on a sensor pack that could be 3D printed then attached by other means like velcro, elastic, or adhesive. Below is one of those first designs. This is getting closer, but still bulky and would feel cumbersome to the patient.
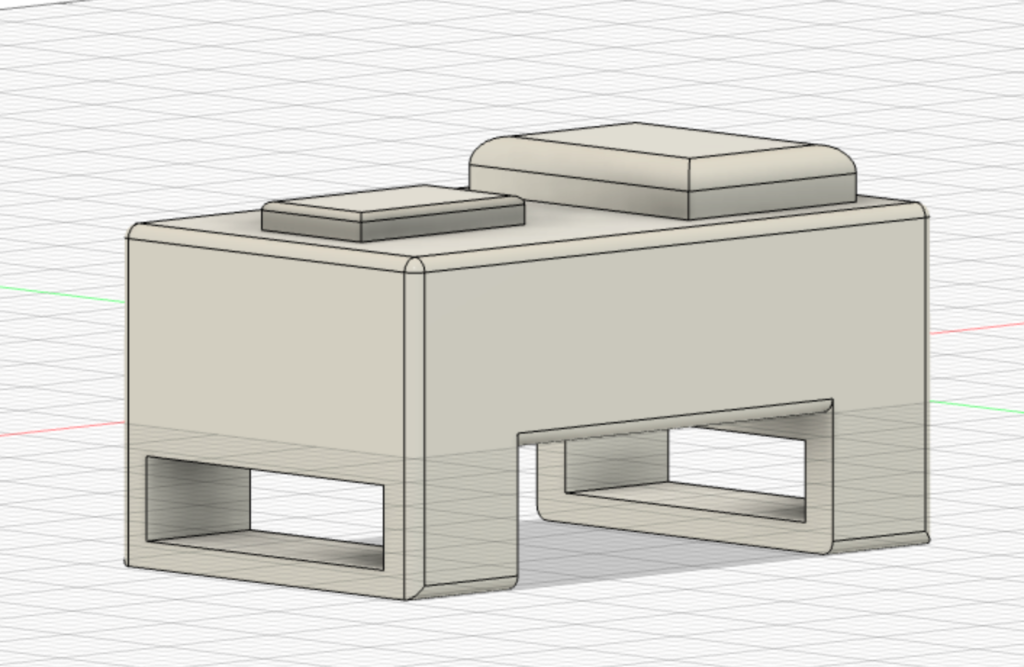
We continued to perfect our 3D printed sensor packs to best fit our team’s electronics and minimize size. Our final prototype is described in the next section.
Final Prototypes


Electronics
There are two electrical components in our prototype: a three axis accelerometer and an Arduino Nano. We have also designed a “works-like” prototype of a buzzer and led component to demonstrate that the alarm will go off once a certain threshold of motion is detected.
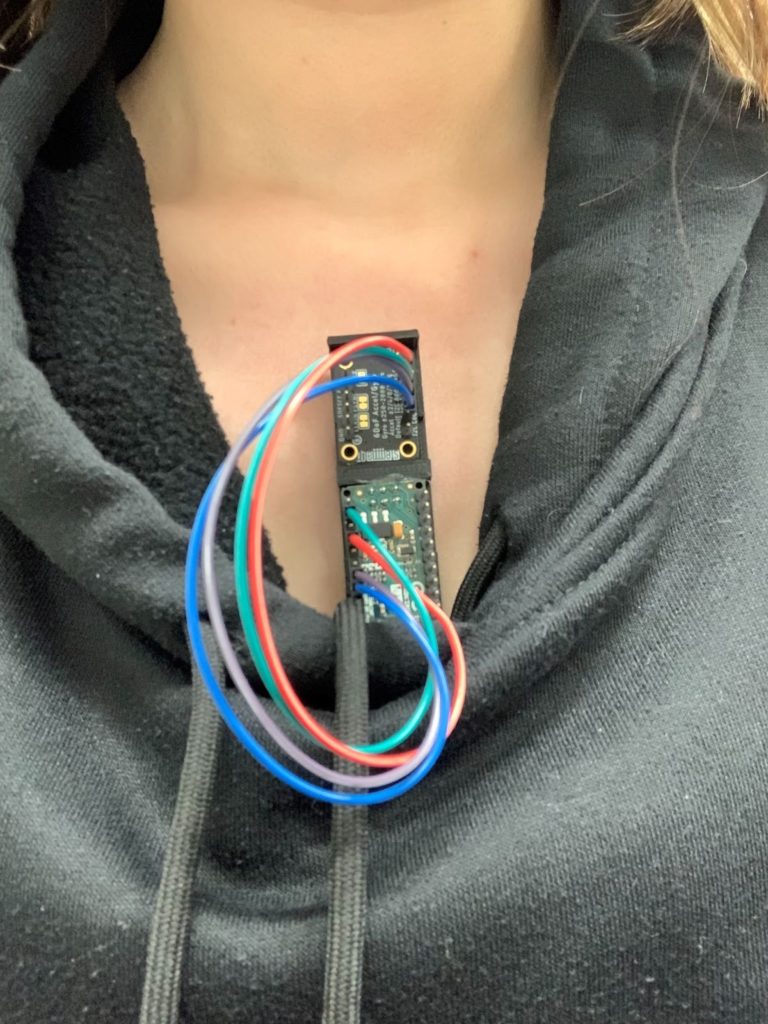
Sensor Pack & Wearable Components
The “sensor pack” is the wearable component that houses the electronics. For our prototype this was 3D printed. The ankle sensor pack is held on with an elastic band, and the chest sensor pack is attached with adhesive. These decisions were made to maximize comfort and durability, and minimize cost.
Patient comfort was prioritized in this component. For this reason, the sensor pack for the ankle is curved, and size is minimized for both the chest and the ankle. In future iterations, size would be furthered minimized since electronics would be customized for this device.
We also kept cleaning procedures in mind. The sensor pack itself is meant to be cleaned with a wipe or standard disinfectant that is already used in hospitals. The elastic bands and adhesives are disposable. For large scale manufacturing an adhesive patch specifically for this device could be developed, similarly to current heart monitors or glucose monitors on the market.
Data Analysis
The team tested this design to gather data and identify patterns that the accelerometer data shows when test subjects performed bed-exit actions. We used MATLAB to interface with the Arduino board. Our sensors can be used to show accelerations in real-time or to store this data for later analysis and calculations. In a clinical scenario real-time data would be used, but recorded data was used to develop the program for detecting the bed-exit.
Future Developments
In future design iterations, the ankle and chest devices will be wirelessly connected to each other, and to the nurses station. The student team chose to leave this to Curbell, because they have more knowledge in this area.
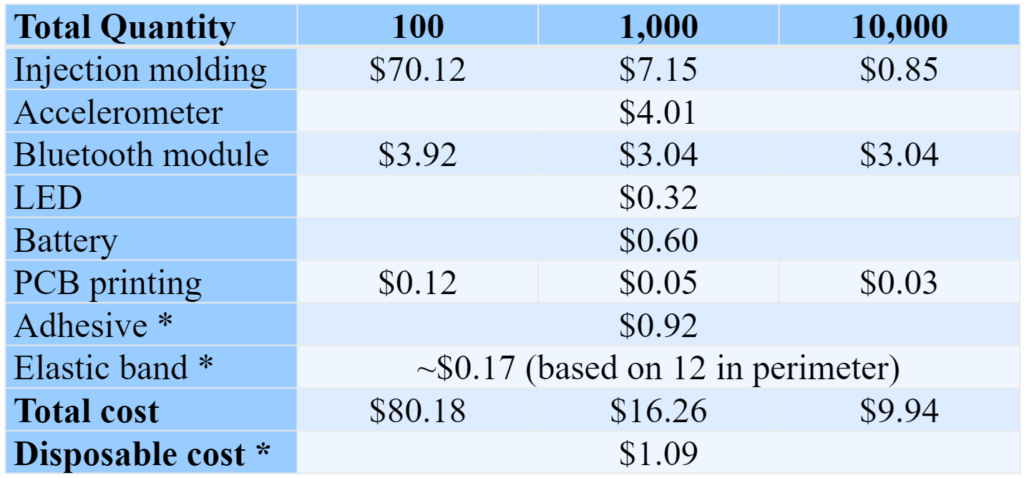
For large scale manufacturing, it would also be best to make customized microcontrollers instead of using the Arduino board used for proof of concept prototyping. Only a few features of the Arduino Nano were used so a smaller microcontroller is both possible and more efficient. Also, the sensor pack would not be 3D printed. Instead a process such as ejection molding could be used and would be more efficient and affordable. Below is breakdown of the cost of manufacturing.
For regulatory impacts on this project, this device would be regulated by the FDA and ISO.10,11 Curbell has already developed a quality system that is certified under both organizations, and any future developments will be done within that system.
References
1. “Fall Management Products.” Curbell Medical.
2. Hitcho, Eileen B., et al. “Characteristics and Circumstances of Falls in a Hospital Setting.”
3. FIS1100. Retrieved 17 April 2022
4. BLUENRG-345AT. Retrieved 17 April 2022
5. NeoPixel Addressable 1515 LEDs (1.5mm x 1.5mm) – 10 pack. Retrieved 17 April 2022
6. LiCB CR2032 3V Lithium Battery (10-Pack). Retrieved 16 April 2022
7. Online PCB Quote. Retrieved 17 April 2022
8. Medical Grade Adhesive Patches. (2022). Retrieved 17 April 2022
9. 1pc Sewing Elastic Band | SHEIN USA. (2022). Retrieved 17 April 2022
10. Center for Devices and Radiological Health. “How to Determine If Your Product Is a Medical Device.” U.S. Food and Drug Administration.
11. “ISO 13485:2016.” ISO.
Acknowledgements:
Special thanks to our professors Dr. Amy Lerner and Dr. Scott Seidman, our teaching assistant and liaison Lucas Lassinger, and our faculty supervisor Veena Ganeshan for their support and guidance in this project. Thank you to Don Gibson, Tom Kennedy, and George Reamsnyder from Curbell for allowing the team freedom to explore design ideas. Thank you to Marcie Metroyanis, RN and DNP, from URMC for giving us insight into the clinical environment.
