Team WorkStress

Customer
Adam Christopher Dziorny, M.D., Ph.D., Physician Scientist, University of Rochester Medical Center
Project Advisor
Edmund C. Lalor, Ph.D. , Department of Biomedical Engineering, University of Rochester
Project Management Liaison
Stella Nantale , CMTI, University of Rochester
Project Background
In an age of increasing demand for healthcare, providing assistance to those who need can take an enormous toll on the healthcare provider. There is a growing importance on preserving the physical and emotional health of caregivers, and identifying strategies to identify workload to combat the toll on caregivers is rapidly gaining attention. Current strategies to measure workload vary. Studies have used surveys (e.g. NASA Task Load Index, Ashgate, 2005) to ask providers or patients their measure of stress or strain in the unit, as well as provider focus groups to ask caregivers their retrospective workload stress. Retrospectively asking providers to recall their workload stress often leads to subjectivity in the measurement of workload stress resulting in measurement errors and unreliable data (Hipp, 2020).
There is no current method for quantifying workload stress in real time. Our proposal is to develop a device that uses an ecological momentary assessment (EMA) to quantify workload stress in the ICU. A EMA is the “repeated sampling of subjects’ current behaviors and experiences in real time, in subjects’ natural environments” (Shiffman, Stone, Hufford, 2008).
Problem Statement
There is currently no method for quantifying and analyzing workload stress in the ICU setting. In order to facilitate data-driven decision-making for the purpose of minimizing workload stress, we aim to address this problem.
Customer Needs
- Assess workplace stress-load in an empirical manner
- Accurately and efficiently store and save stress data
- Device is secure and does not identify users
- Device should be able to be used quickly
Customer Wants
- Device must be small and unobtrusive
- Device gives feedback to user after a button-push
- Device can be powered by batteries
Prototyping
Prototype 1 – Breadboard
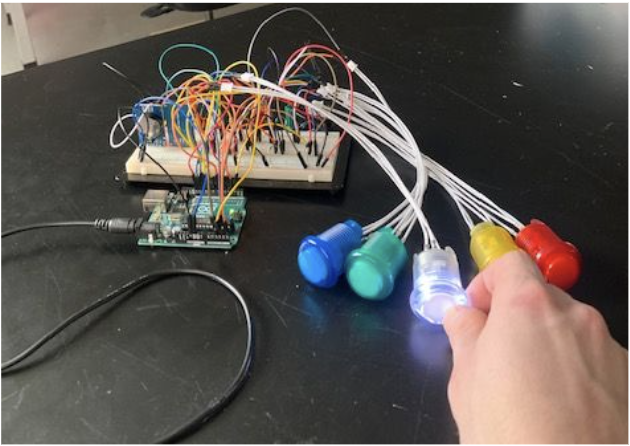
Above is our working breadboard model, which served as our first prototype. Once this was completed, we worked to translate it to a Printed Circuit Board (PCB), which is far more robust and less prone to random errors due to loose connections.
Prototype 2- First PCB
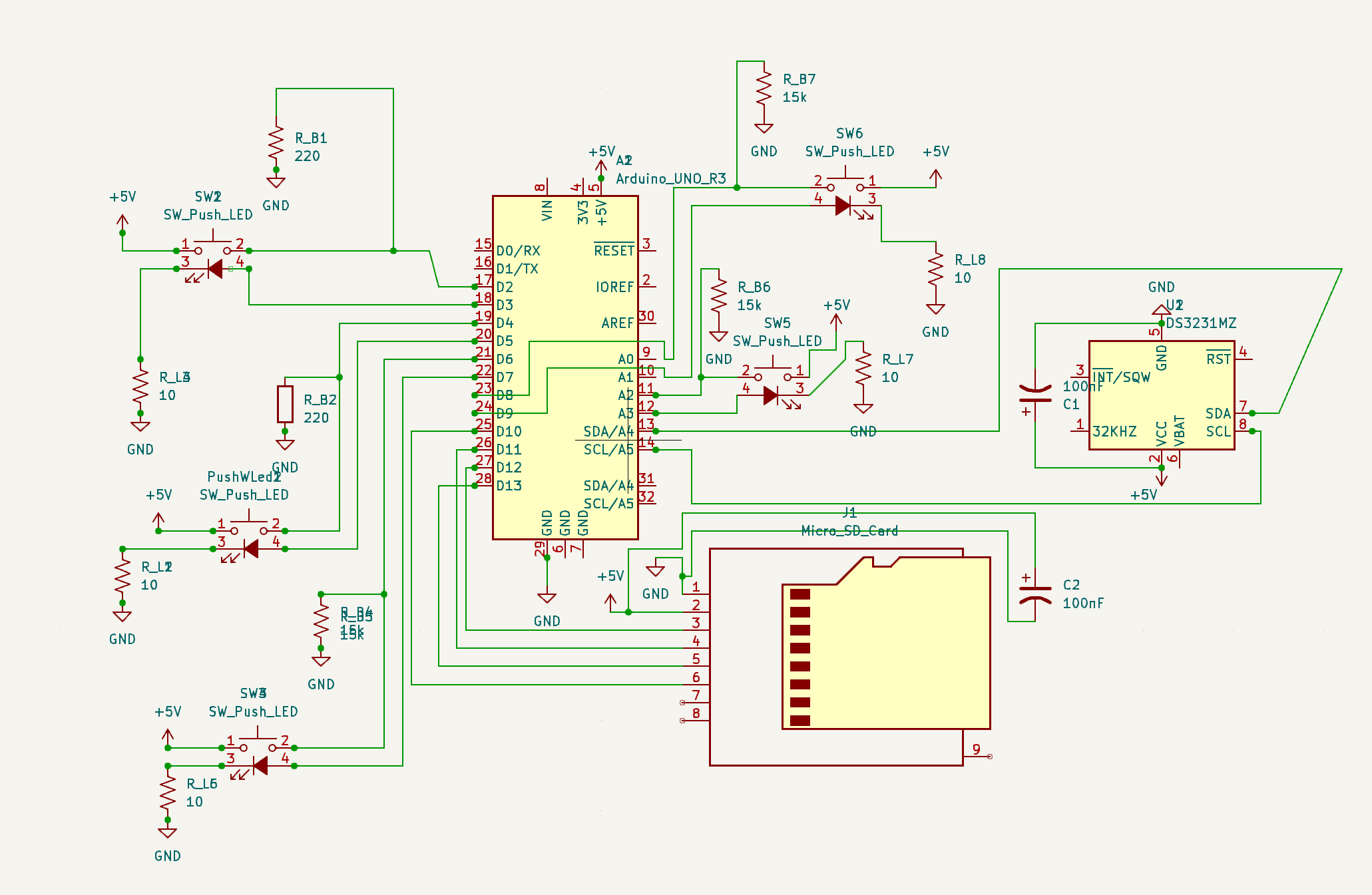
Our first PCB had two major design flaws. First, a button was double grounded in the schematic by accident rendering it useless. Secondly, we diverted from our breadboard design by adding two decoupling capacitors as it was good practice to have them; unfortunately, these decoupling capacitors impeded our button functionality further revealing another flaw.
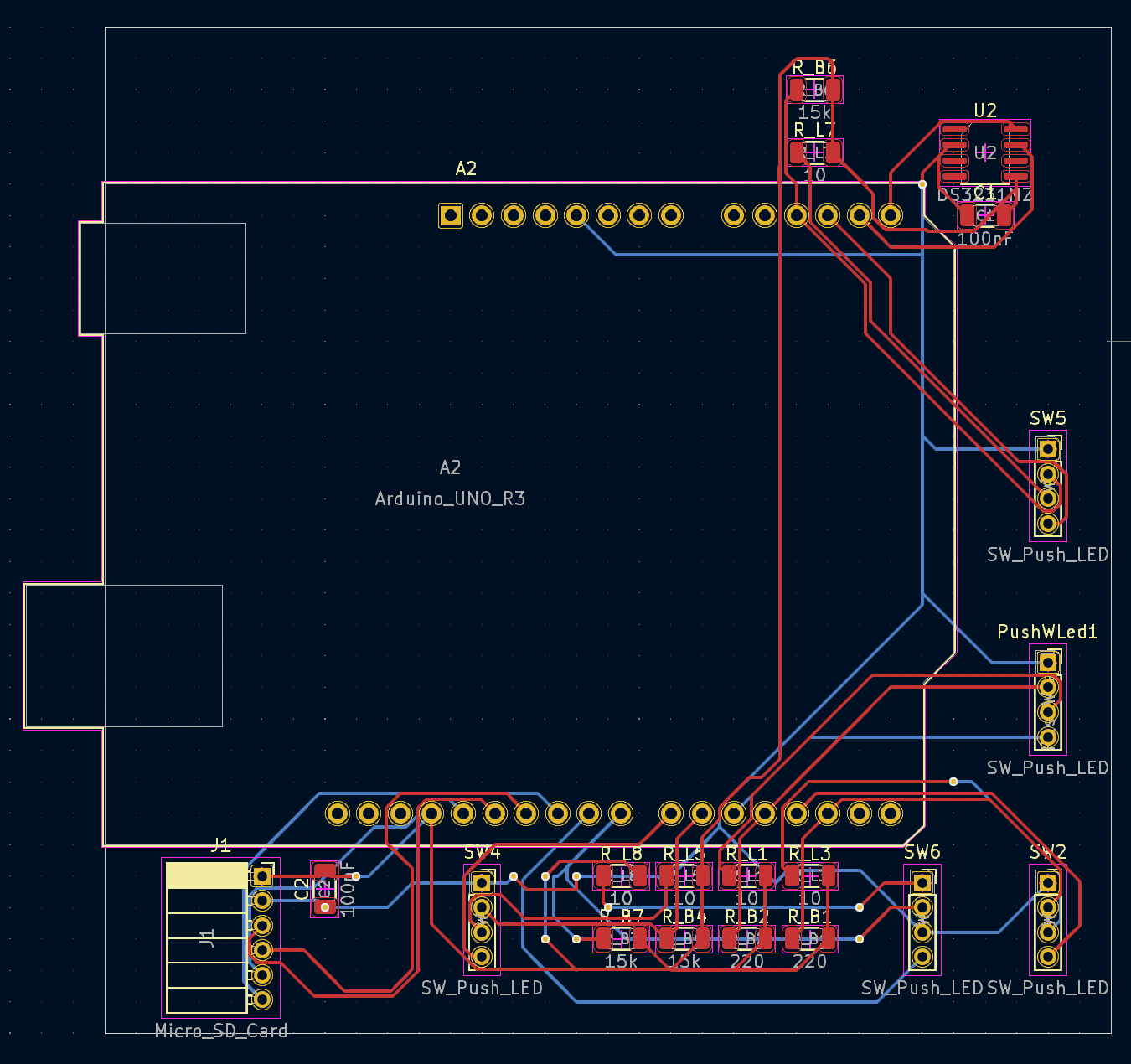
Prototype 3- Second PCB
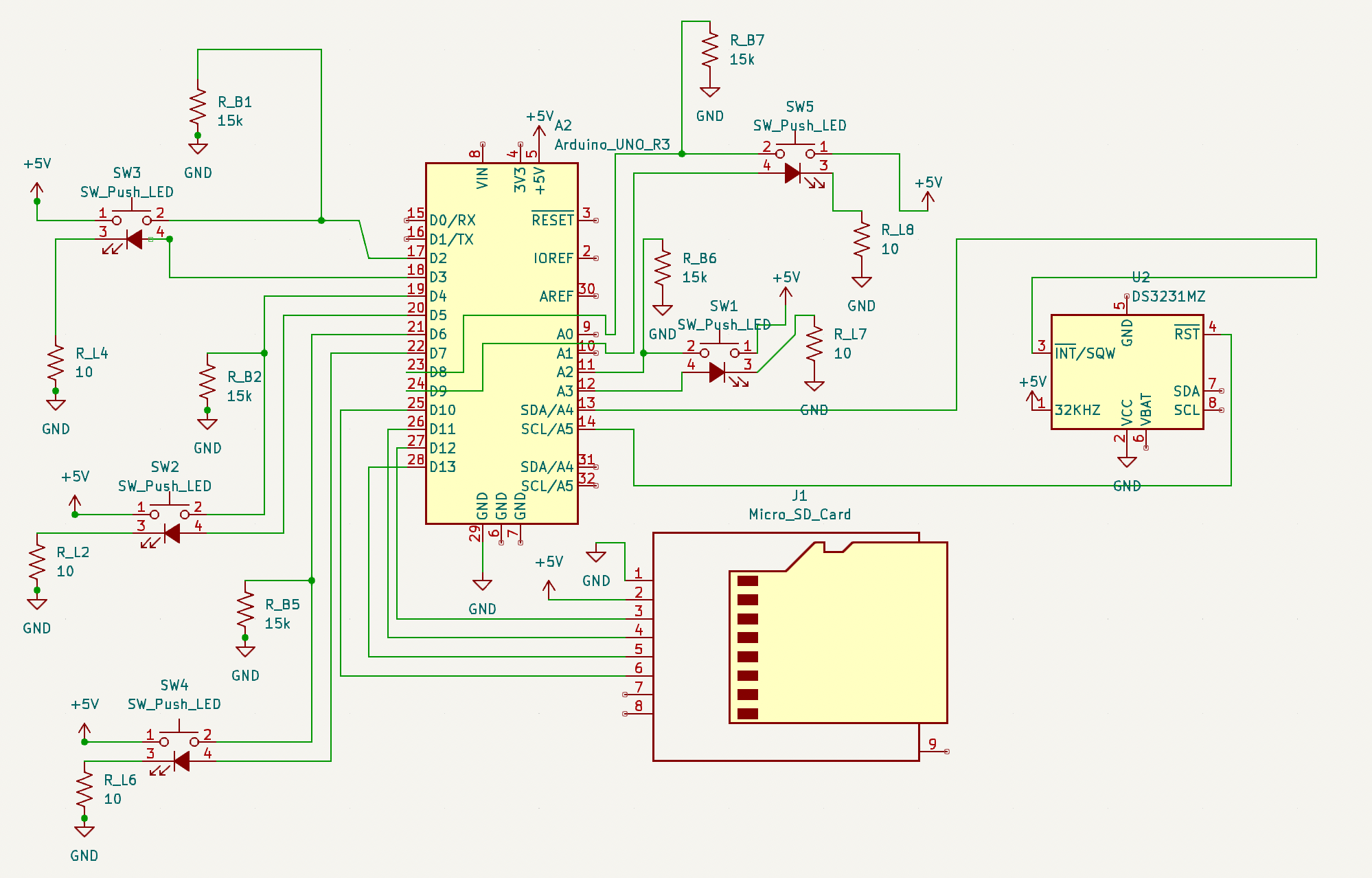
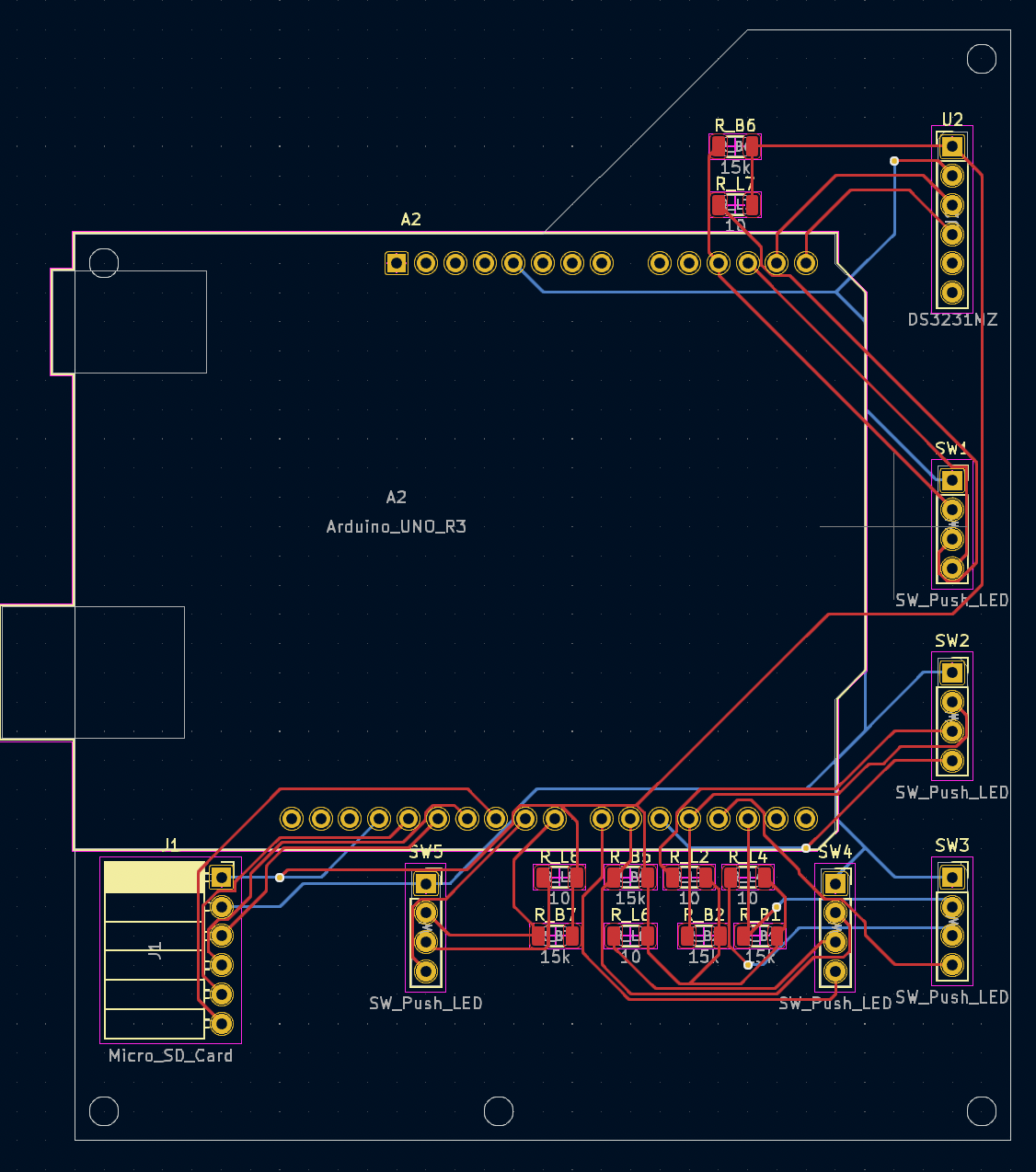
Our second PCB design fixed the flaws in the first design and polished the design of the PCB. The button orientations were reorganized into a manner making all button inputs the same, we fixed the double grounded button , and removed the capacitors. Additionally, we made wire traces bigger, added screw holes to our PCB to screw into our scaffold in the project box, and made the real time clock module through-hole mounted. Now the only difference between our initial prototype and final device is the modality (breadboard → PCB).
Final Device Demo
Design Evaluation
Technology Acceptance Model (TAM)
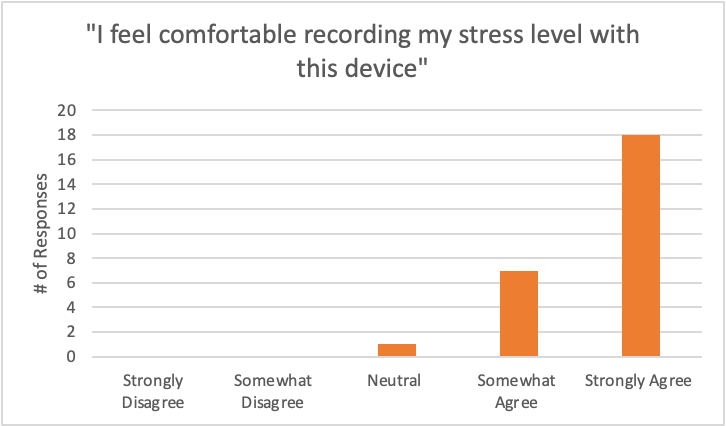
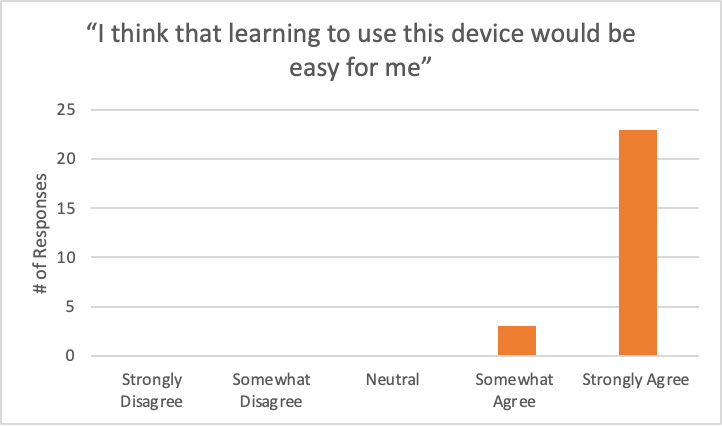
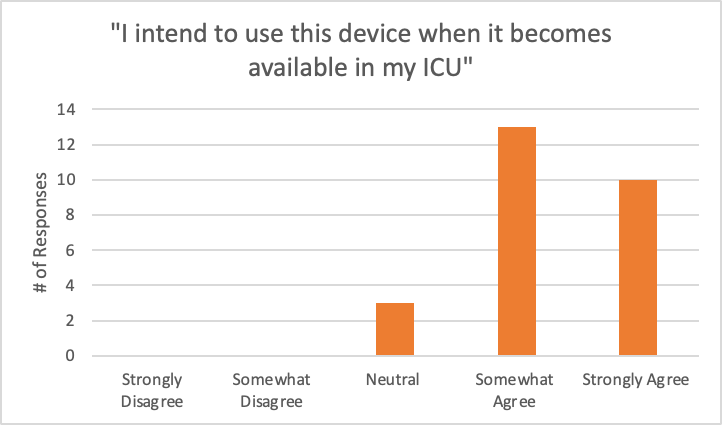
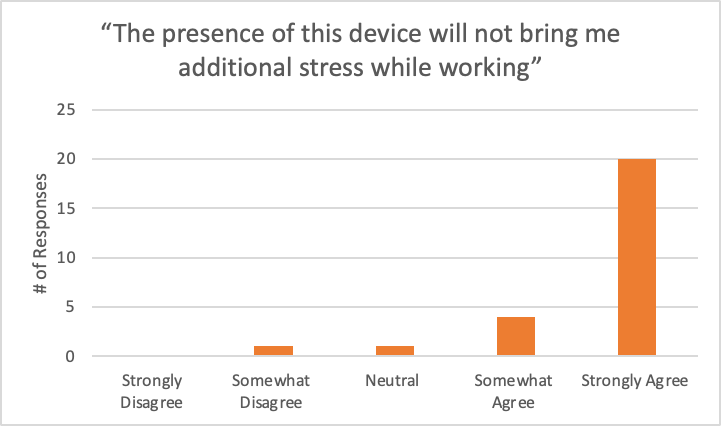
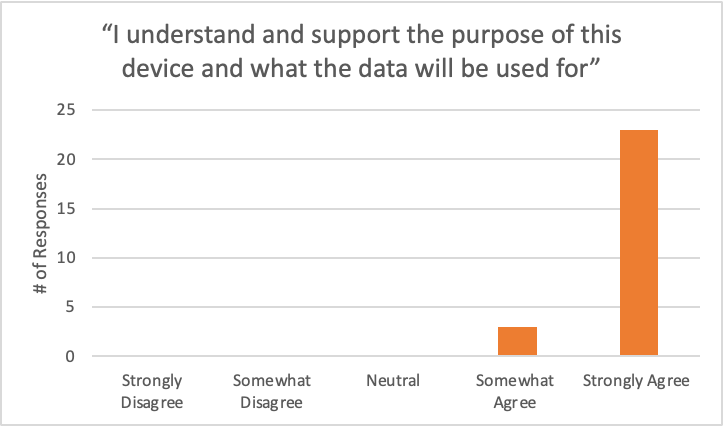
In order to evaluate our device, we utilized an adapted version of the Technology Acceptance Model (TAM), which aims to measure how end-users (in this case, the healthcare workers who will be recording their stress) view the perceived usefulness and ease of use of a device.Perceived usefulness refers to the user’s belief that the technology will enhance their job performance or make their life easier, while perceived ease of use refers to the user’s belief that the technology is easy to use and understand.(M.Nguyen et al. 2020)
We created a simple, five question survey in order to assess the perceived ease of use and intention to use our device. In order to get a measure of perceived usefulness, we gave a thorough description of the research project prior to administering the survey. Sample questions of our survey are shown below:
- I feel comfortable recording my stress level with this device.
- I think that learning to use this device would be easy for me.
- I intend to use this device when it becomes available in my ICU.
- I understand and support the purpose of this device and what the data will be used for.
- The presence of this device will not bring me additional stress while working.
Nurses were asked to rate their level of agreement with the above questions on a 5 point scale from Strongly Agree to Strongly Disagree.
Evaluation Results
Future Directions
As of now, we have delivered on what the customer wants and have a fully functional EMA device that can be used for his research project. The device is easy to use and easy to interact with. However, there are ways to improve our design. Using a less power-intensive microcontroller could facilitate making the device battery powered. This can alleviate the problem that the device must be plugged into an outlet to function, which takes up valuable outlet space in the pediatric ICU.
As for the next steps in the research project, we recommend taking a machine-learning based approach in which electronic health record data is associated with the stress data, with the stress data being used as the “ground-truth” for the model. With enough data, this can lead to a comprehensive model with which simulations can be run of different scenarios in the ICU, with which managers can determine what to change to obtain the least stressful environment.
Acknowledgements
- Customer: Dr. Adam Dziorny
- Project Advisor: Dr. Edmund Lalor
- Project Management Liaison: Stella Nantale
- Dr. Scott Seidman
- Dr. Michael Giacomelli
- Martin “Marty” Giras
- Laura Henry
- Marica Kerr
- Joshua Fox
