
Team Members

Mentor
Dr. Richard E. Waugh, PhD, Biomedical Engineering, University of Rochester
Lucas Lassinger, CMTI Student, University of Rochester
Customer
Dr. Sara Salim, MD, Department of Physical Medicine and Rehabilitation, University of Rochester Medical Center
Problem Statement
Current posture modification devices that decrease duration of bowel movement are not suited for achieving and sustaining the squatting position for individuals with neurogenic bowel (NB).
Background & Customer Scenario
Neurogenic bowel dysfunction is a condition that affects individuals with severe neurological conditions, and it is defined as the loss of normal bowel function. For individuals with NB, performing a bowel movement can be a time consuming process and often requires a bowel program, which is an individualized and complete plan for NB patients that helps them accomplish a bowel movement. According to an interviewed caregiver of an individual with NB, the bowel movement may take up to 2-3 hours per session, and this session can occur typically 3-4 times per week (Stiens 1997, Caregiver VoC). This arises diverse physical, psychological and social effects, such as the time consuming nature of the procedure, the prolonged time spent sitting in one position which can lead to pressure ulcers, as well as limited control of their bowel movement. Posture modification devices are popularly used to reduce the duration and potential strain involved with performing a bowel movement, but most of these defecation posture modification devices target individuals with a full range of motion. Therefore, our goal is to create a posture modification device that allows an individual with NB to safely achieve a squatting position for the duration of the time it takes for them to perform a bowel movement.
The ideal patient we will consider for our design situation is an individual with a T12-level spinal injury, which falls under the category of ASIA A. This refers to somebody who has no motor or sensory function below the thoracic section of the spine, however maintains much of their upper trunk function, and can hold their posture upright for extended periods of time. We expect that by targeting the most severe injury classification, individuals with less severe injuries will be indirectly taken into consideration. Thus, a wide range of individuals with NB could benefit from our device.

Design Concept & Prototyping
Design specifications were developed with input from our research team team as well as our customer Dr. Salim. The VoC interviews with a caregiver and trainer of the bowel care process, NM, and OT specialists provided expertise into the metrics for these design specifications. The design specifications must comply with the standards: ANSI RESNA WC-1 and ISO Standards 7176, and 17966. Our customers asked us to focus on creating a model complying with three critical quality requirements: (1) Posture Modification, (2) Patient Safety, and (3) Convenience.
(1) Posture Modification
- The system must support a 22.5°-35° hip flexion angle for the user. (Dr. Salim; Sakakibara 2010)
- The system must support the desired hip flexion angle within a timeframe between 2-3 hours. (Stiens 1997; Caregiver VoC)
- The system must provide a circular hole of 38-40 square meters for perianal region surface area access. (Nurse VoC; OT VoC)
- The system must provide 5.5-6.0 inches L by 14.25-16.25 inches H user under hand seat access from the front. (Malassigné 2001; Nurse VoC; OT VoC; HOMCOM Accessibility Commode Wheelchair, Amazon)
- The system must provide 17.5-21.25 inches W by 14.25-16.25 inches H user under hand seat access from the back. (Malassigné 2001; Nurse VoC; OT VoC; HOMCOM Accessibility Commode Wheelchair, Amazon)
(2) Patient Safety
- The system shall support 300 lbs of weight. (Caregiver VoC)
- The system must comply with the cleanability requirements of ISO standards ISO 17966: 2016.
- The system shall provide resistance to water in the IP range between IPx4 to IPx5. (Fogg 2021)
- The system shall operate within a relative humidity range of 0 to 60%. (Hussain 2018)
- The system shall operate within a temperature range of 40 to 120 degrees Fahrenheit. ( ADA accessibility standards)
- The system shall provide user:
- Ischial tuberosities contact pressure in the range of 0 to 40mmHg per 15 to 20 minutes.
- Trochanters pressure in the range of 0 to 60mmHg per 15 to 20 minutes
- Sacrum contact pressure in the range of 0 to 19mmHg per 15 to 20 minutes
- Coccyx contact pressure in the range of 0 to 19mmHg per 15 to 20 minutes
(Ferguson-Pell 1990; Agrawal 2012; Nurse VoC; OT VoC)
(3) Convenience
- The system must fit within a 16 to 18 inch distance from the centerline of the toilet (ADA 2010)
- The system must provide 0 inches of slip from the commode/shower chair external system (Dr. Salim; Caregiver VoC).
- The system shall provide 0 inches of slip from the ground of the external system environment. (Malassigné 2001; Nurse VoC; OT VoC)
- The system shall not tip in the directions of forward and backward on a 10 degree incline, and sideways on a 5 degree incline plane (ISO 17966; Malassigné 2001; Nurse VoC; OT VoC)
- The system shall account for adjustable dimensions to accommodate differences in:
- Sitting height (device upper angle bar range): 8.3 to 10.8 inches
- Thigh clearance (seat surface to top of thighs): 4.4 to 7.5 inches
Our device consists on a torso-lean attachment meant to be connected to the HomCom Commode Chair(HomCom Personal Mobility Assist Waterproof Commode Shower Wheelchair Self-Transport Cart, 2022). The device development was divided into three subsystems: (1) User to Device Interface, (2) Posture Modification, and (3) Device to Environment Interface.
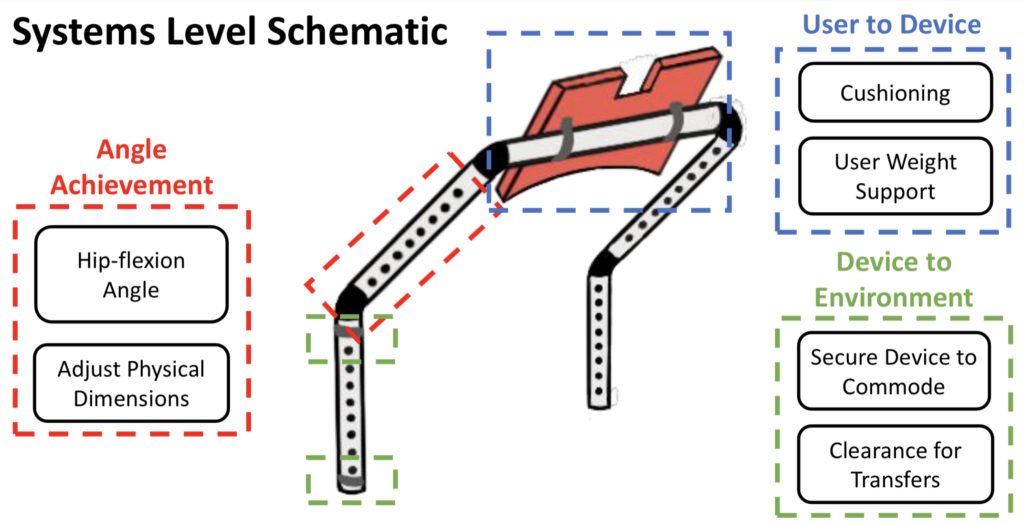
The device is composed as follows:
- (1) There are two vertical bars, one on each side of the commode, with adjustable dimensions that will be attached to the commode via clamps.
- (2) These adjustable bars then attach to a bar fitting socket, which allows the user insert and remove the support bar in order to accomplish transfers and clearance of the device.
- (3) The fit socket is then attached to another set of bars with adjustable dimensions. This set of adjustable dimensions allows the user to move the cushion closer/further away, and thus move the cushion higher/lower on the user’s torso.
- (4) A single horizontal support bar connects the bars, allowing more structural stability for more interface to connect with the cushion.
- (5) The horizontal support bar interfaces with a cushioned chest support connected by U-clamps which will interface with the user’s torso.
- (6) Anti-tipping bar is a rotatable clearance mechanism that interfaces with the bottom commode bar via a T-connector clamp to account for user safety and provide additional stability.
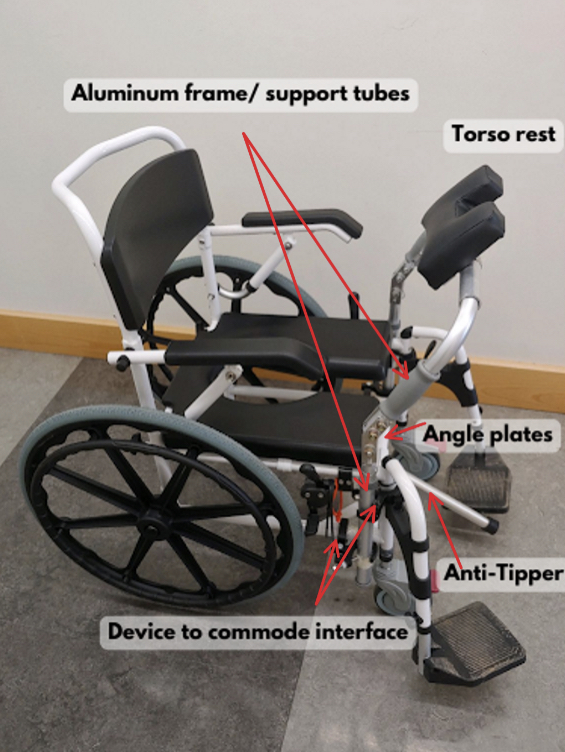
Final Prototype

Testing & Results Assessment
Our design process began with mechanical testing of attachment and interface materials to select secure attachment mechanisms, and determine which materials had mechanical properties most appropriate for compatibility with the HomCom commode chair as well as durability for sustaining the user and its intended medical use. After testing several materials and methods, we were able to finalize material selection and create more prototypes with the aim of reflecting a realistic feel of the torso-lean device overall. Through multiple in-person and virtual meetings with our customers, we were able to evaluate our prototype and receive helpful feedback.
To quantify whether our torso-lean device could accomplish completion of the key aims we focused on, we performed a series of tests, as described below.
Anthropometric Angle Calculation
Anthropometric calculations were conducted in Matlab to determine the required fixed angle for the lower and upper vertical bars, as well as the adjustment dimensions for 5th, 50th, and 95th percentile users. This is to be within the desired range of the 22.5-35 degree hip flexion angle.

Support & Sustain Squatted Position
The method for testing the sustained squatted position required the use of 3D Slicer (an open source software that can be used for image analysis and visualization). The sustained squatted position hip flexion angle was measured as a function of time. Each team member underwent a test in which the device is locked at the desired hip-flexion angle with the user resting on the torso cushion. The hip flexion angle was measured with respect to three points on the body and assessed every ten minutes for a total of 1 hour. This testing plan provided insight into the structural stability of the framework, as well as the anatomical support the torso cushion and leaning forward position can both provide for the user. In addition to the quantitative analysis regarding displacement of the anatomical regions, a qualitative analysis was performed to determine modifications required for longer durations of device use.

| User | ICC Value | Pearson Coeff. |
| Jack | 0.88 | 0.95 |
| Chas | 0.59 | 0.61 |
| Maddi | 0.75 | 0.95 |
| Alex | 0.83 | 0.90 |
| Cami | 0.83 | 0.93 |
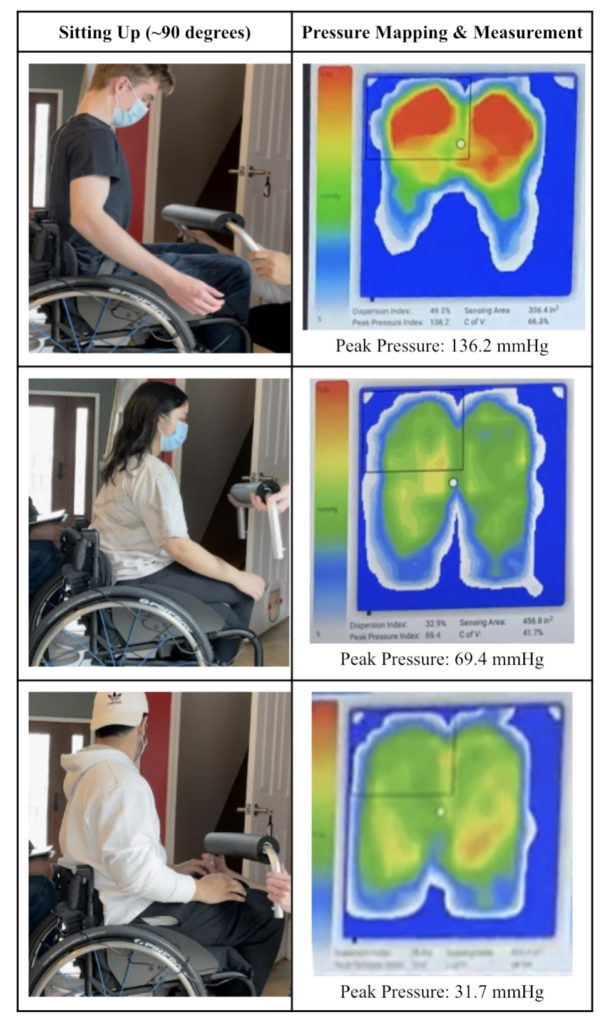
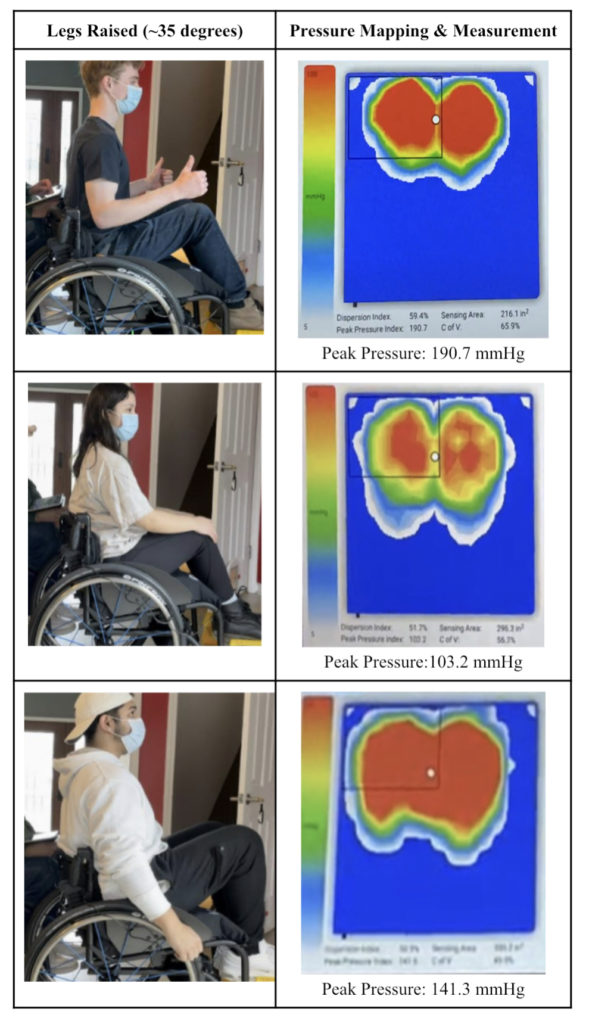
User Contact Pressure Mapping
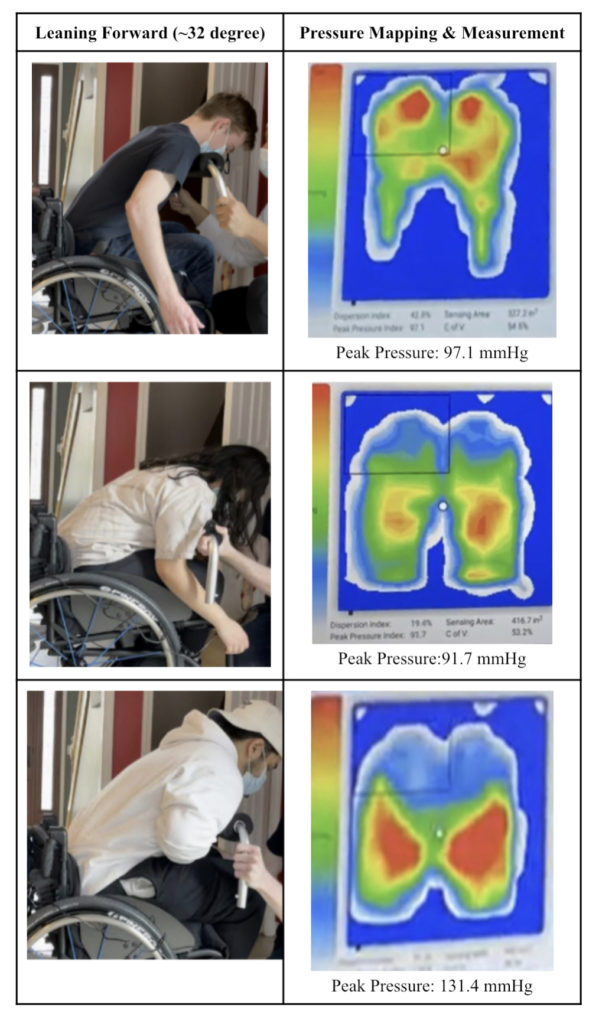
A key concern regarding the use of a angle generation device was being able to reduce pressure in areas with tendency to develop pressure ulcers, specifically at the ischial tuberosities. Testing was conducted in three different individuals of different dimensions and weights at three positions (1) Sitting up ~90 degrees, (2) Legs raised ~35 degrees, and (3) Leaning forward ~32 degrees. This allowed us to assess the pressure distribution of our design concept, and confirm the viability of safely redistributing the pressure to decrease concern for ulcers.
(1) Sitting up (~90 degrees)
(2) Legs raised (~35 degrees)
(3) Leaning forward (~32 degrees)
Tipping Analysis
Due to the usage of the device involving leaning forward, a tipping analysis was conducted to ensure safety. This was done with two varying cases in the forward lean position:
- Case 1: An individual sitting properly in the commode chair scooted all the way towards the back, and sitting halfway from the front of the commode chair.
- Case 2: Adding a 35 lb weight to the torso for the first case.
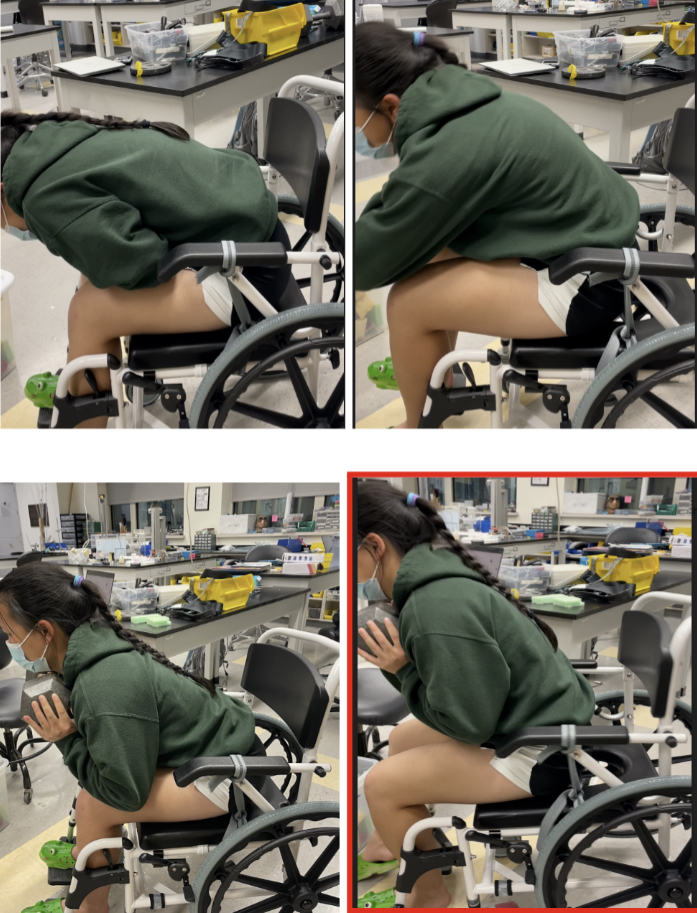
Without the weight, the commode chair did not tip over in Case 1. As for Case 2, the commode chair began to tip over as shown in the bottom right image, outlined in red. Therefore, Case 2 indicates a worst-case scenario: an individual sitting halfway on the commode chair and leaning fully forward. This concluded the decision to design an anti-tipper that can interface with the ground.
Future Directions
Our device is currently at a stage in which further simplifications can be made. First, the 60 degree bent bar generating the 22.5-35 degree hip flexion angle could be made into a single bar piece (fully eliminating the angle plate) to reduce the risk of skin tears as well as manufacturing costs. Second, limitations of arm movement and reach for individuals with broad shoulders can be addressed by lowering the horizontal bar and incorporating a slide board mechanism for the torso cushion. As for testing, the support user weight testing plan would ideally be repeated to ensure that the clamps prevent moments from occurring or assessing the need for incorporating additional bars interacting with the floor and acting as counterweight to prevent the rotation. Furthermore, we would like to conduct other testing plans that were unable to be done, such as humidity and moisture resistance testing, as well as temperature testing. Another design change that may be implemented in the future is the incorporation of the anti-tipper attachment, and a forehead rest.
Our team has participated in a couple of business/design competitions. Throughout our conversations with our advisor, we have considered business planning with regards to design/utility patents. This is something that has remained as an open conversation, but we are first focusing on simplifying our design. Next steps also include clinical testing as briefly discussed with our customer. The concept challenge was brought to us with an intuition that the squatting position is also capable of assisting individuals with spinal cord injuries to produce an easier bowel movement. However, this step may solely be organized by our customer or her colleagues at URMC.
Acknowledgements

