Noninvasive, real-time blood glucose monitoring for telehealth patients
Design Team: Maryah Albahar, Lalana Appasani, Isobel Bond, Kevin Segarra Valentín, and Ashlynne Xavier
Supervisor: Dr. Benjamín Castañeda, Professor of Biomedical Engineering, Professor of Electrical and Computer Engineering, University of Rochester
Customer: Dr. José G. Pérez Ramos, Assistant Professor of Public Health Sciences, University of Rochester Medical Center
Problem Statement
A non-invasive wristband device that utilizes a photoplethysmography (PPG) sensor has been developed to provide accurate, real-time estimates of blood glucose levels. The project aims to design and prototype the device, extract reliable physiological signals, and develop a signal processing algorithm to correlate PPG data with blood glucose levels, ultimately supporting easier and more consistent diabetes management.
Background
In remote areas like Vieques and Culebra, small sub-islands of Puerto Rico, limited access to specialized healthcare exacerbates the impact of widespread diabetes2,4. Most residents rely mainly on telehealth for communication with physicians and disease management. Traditional blood glucose level (BGL) monitoring methods are invasive and uncomfortable, which discourages consistent use and further adds to difficulties in diabetes management3. Photoplethysmography (PPG) is a common noninvasive method of measuring changes in blood volume and makeup using emitted light, and has shown some promise in estimating BGL. Our initial algorithm builds on the work of Hammour & Mandic (2023), who found that average peak widths and heights in PPG signal cycles correlate with blood glucose levels5. Using raw PPG data from our device, we identify the 10 most consistent signal cycles, calculate their average height and width, and validate algorithm consistency to estimate glucose levels. This project sought to address these difficulties in BGL monitoring and patient-physician communication through a wrist-worn PPG-based device, a signal processing algorithm to estimate BGL ranges, and a graphical user interface (GUI) to display and communicate current and past readings.
Design Specifications
Patients, healthcare providers, and community health workers in remote or under-resourced areas, such as Vieques and Culebra, need a glucose monitoring solution that is non-invasive, user-friendly, and reliable. To meet these needs, the device must provide accurate readings of blood glucose levels across diverse patient populations and feature an intuitive, easy-to-navigate user interface. Portability and durability will be an inherent advantage of the device design and are essential along with the device’s ability to deliver results quickly. Its successful integration into existing healthcare systems will depend on comprehensive health education materials distributed through local community health workers. Affordability is also a key consideration to ensure adoption in underserved regions but will be continuously improved upon through future iterations of development.1 Additional features such as high weather resistance, remote communication with healthcare providers, and adherence to HIPAA data privacy standards will only further enhance the device’s utility.
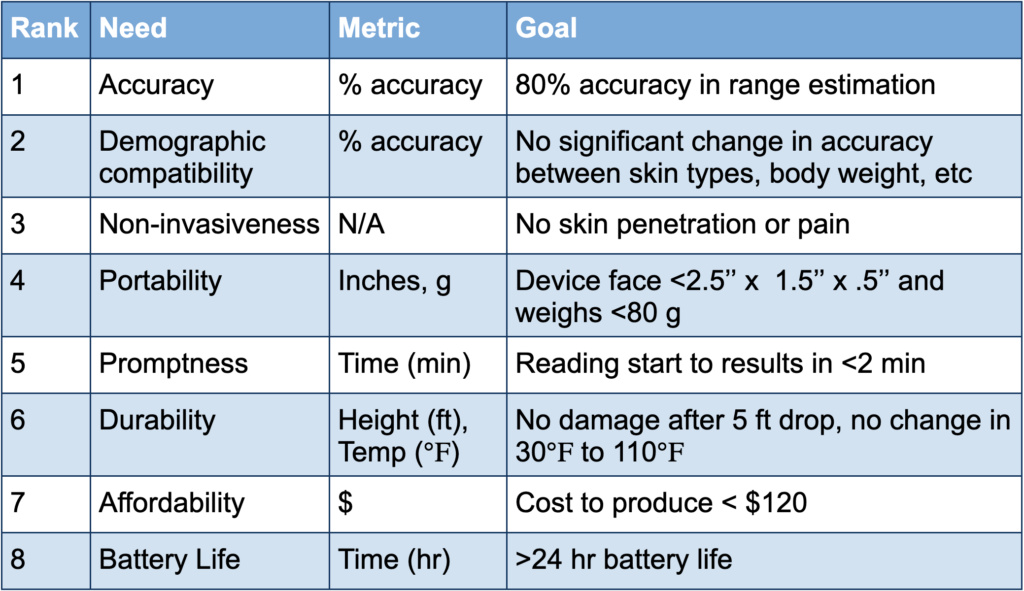
Table I. Customer needs for the device. Needs are ranked along with metrics and goals.
Design Concept
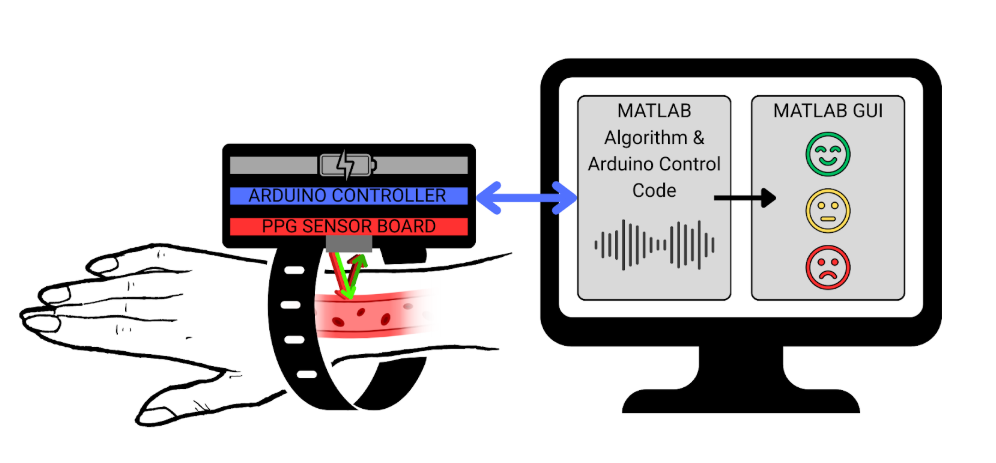
Figure 1. Overall design concept of the wearable PPG-based wristband, algorithm, and GUI. The wristband contains the PPG sensor for data acquisition, Arduino for communication with the computer, and battery. Signal processing and the GUI are both done in MATLAB.
User Interface
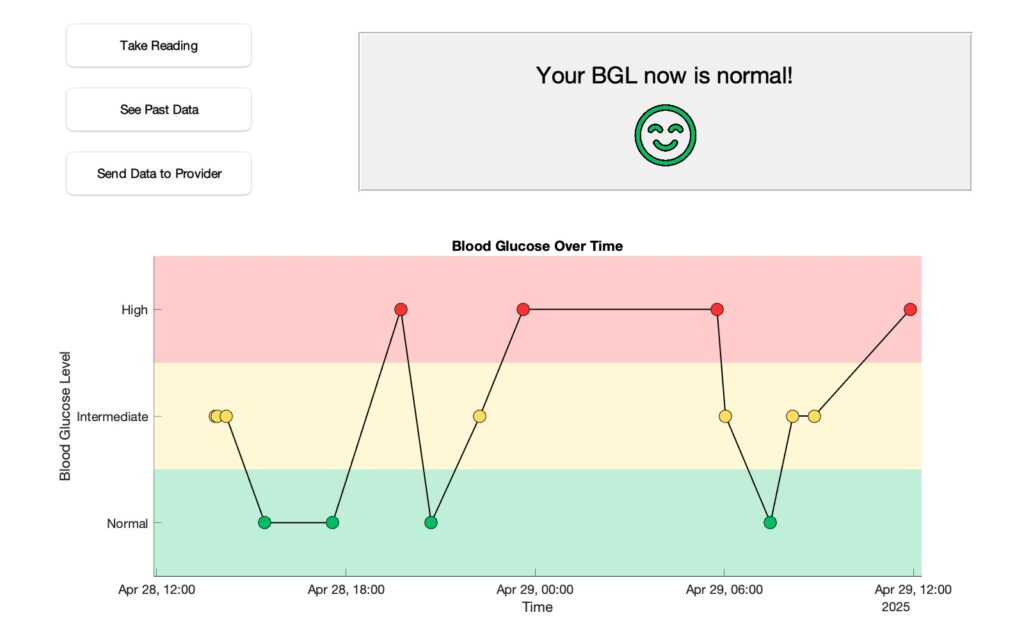
Figure 2. MATLAB prototype of the GUI. Users can get real-time data, with the current reading displayed on the top right, and view readings from the past 24 hours on the graph. Ranges (in mg/dL): “Normal” <100, “Intermediate” 100-140 , “High” >140.
Future Directions
Future iterations of development will focus on improving the device’s accuracy, durability, sustainability, and accessibility1:
- Expansion of the algorithm to improve accuracy, including use of other signal features, expansion of calibration testing, greater testing on individuals with diabetes, and machine learning
- Climate-resistant hardware
- Long battery life
- Reusable energy integration, such as solar power
- Multilingual user interface
- Bluetooth communication between the wristband and computer
- Remote communication with healthcare provider database
- Comprehensive health education materials for global scalability
Acknowledgements
Thank you to our customer, Dr. José G. Pérez Ramos, for identifying the need for this device and offering valuable feedback throughout its development; our supervisor, Dr. Benjamín Castañeda, for his ongoing support and expert guidance during the design process; our professor, Dr. Scott Seidman, for his dedication and instruction throughout the semester; our project management liaison, Jack Zapp, for his support and insightful feedback; and our senior laboratory engineer, Martin Gira, for his assistance with 3D printing and his guidance during product assembly.
References
- Access to medical devices in Low-Income countries. https://www.chausa.org/news-and-publications/publications/health-progress/archives/september-october-2018/access-to-medical-devices-in-low-income-countries.
- Colón YMS, Pérez EA, Rivera MLR, et al. Community forums as amplifiers of communities’ voices: Isolated communities in Puerto Rico. International Journal of Environmental Research and Public Health. 2023;20(14):6335. doi:10.3390/ijerph20146335
- Frontino G, Meschi F, Bonfanti R, et al. Future Perspectives in Glucose Monitoring Sensors. touchREVIEWS in Endocrinology. 2010;9(1):21. doi:10.17925/ee.2013.09.01.21
- Tierney EF, Burrows NR, Barker LE, et al. Small area variation in diabetes prevalence in Puerto Rico. https://pmc.ncbi.nlm.nih.gov/articles/PMC4537060/. Published June 1, 2013.
- Hammour, G., & Mandic, D. P. (2023). An In-Ear PPG-Based Blood Glucose Monitor: A Proof-of-Concept Study. Sensors, 23(6), 3319. https://doi.org/10.3390/s23063319
