An assistive cycling device to allow mobilization of bed-bound patients in the ICU.
Background and Problem Statement
- More than 5 million people are admitted to ICUs in US/year1
- Immobility during ICU stays leads to complications2: including
- ICU-acquired weakness
- Long-term disability
- ICU-associated delirium
- Higher rates of mortality
- Longer ICU stays
- In-bed cycling ergometry is a safe and effective intervention for ICU patients3, 4
- Early mobilization has been found to:
- Decrease one-year mortality rates5
- Decrease prevalence of psychiatric conditions after ICU discharge
- Improve hyperglycemia7
Problem Statement: ICU patients who are unable to leave their beds without assistance may benefit from increased access to mobility; however, the time required for ICU PTs to exercise patients frequently and the cost of current in-bed cycling ergometers pose a barrier to improving patient outcomes. We are tasked with creating a device that allows patients to move through an assisted cycling motion with their lower limbs from bed at a more accessible price point, allowing patients to reap the benefits of early mobility without needing to be able to leave their beds.
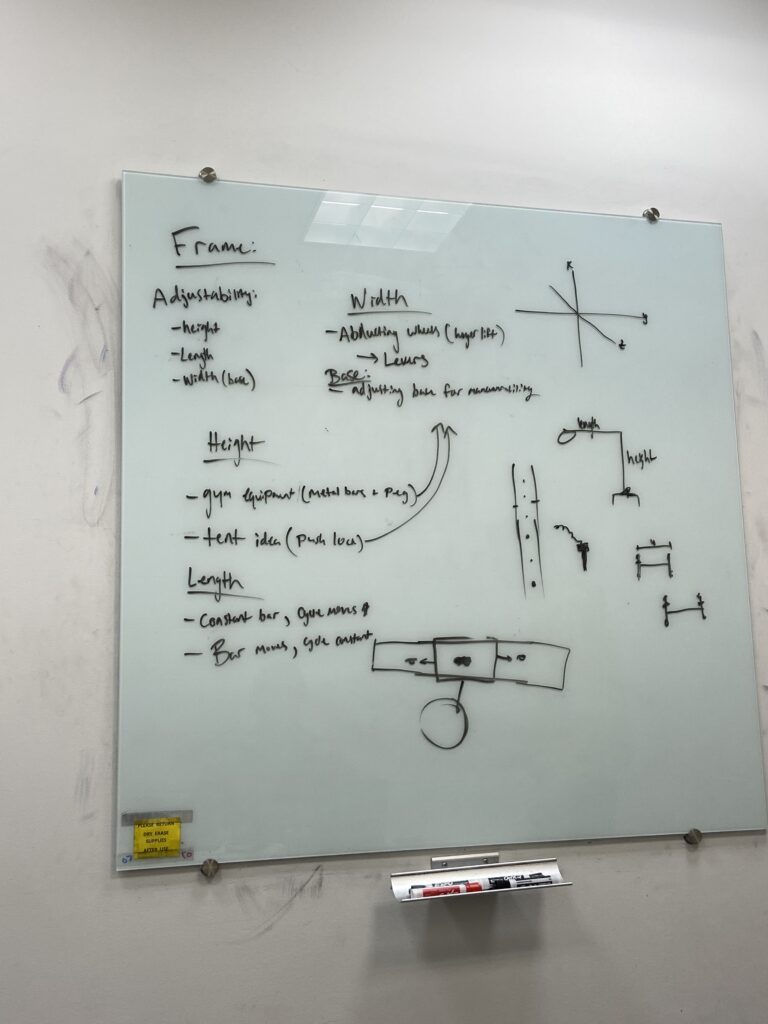
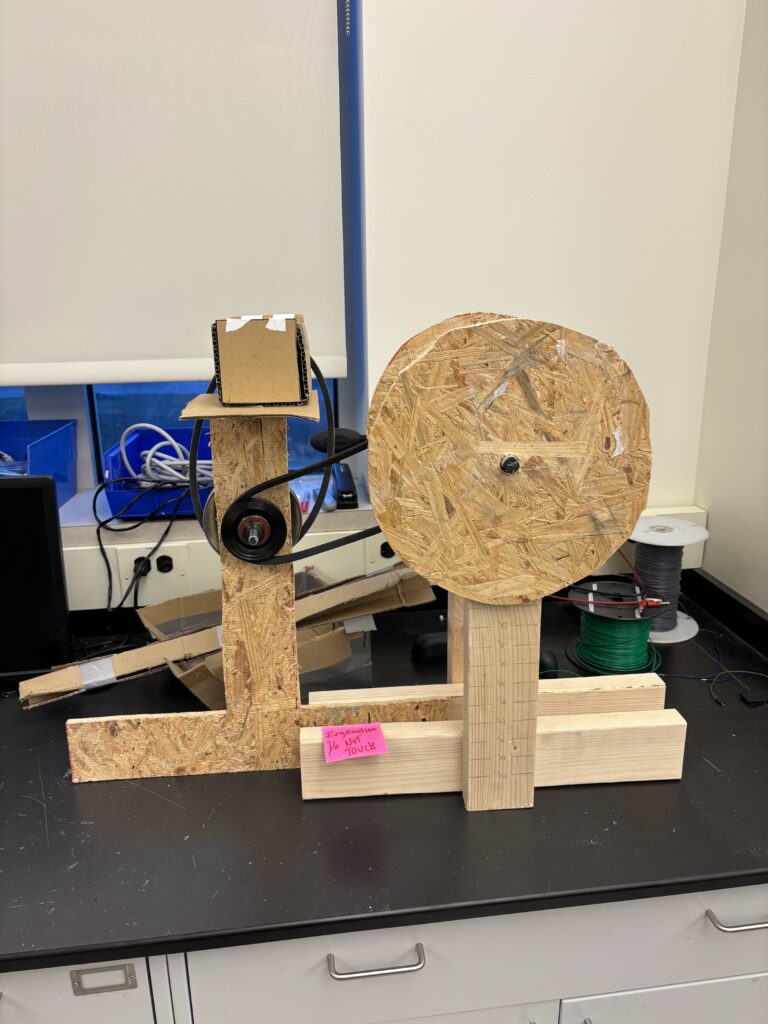
Design Process
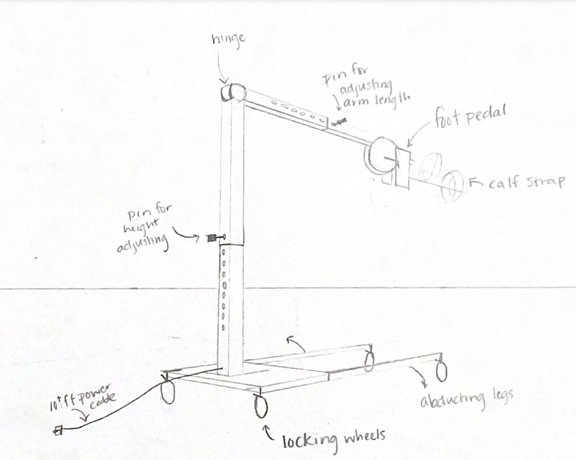
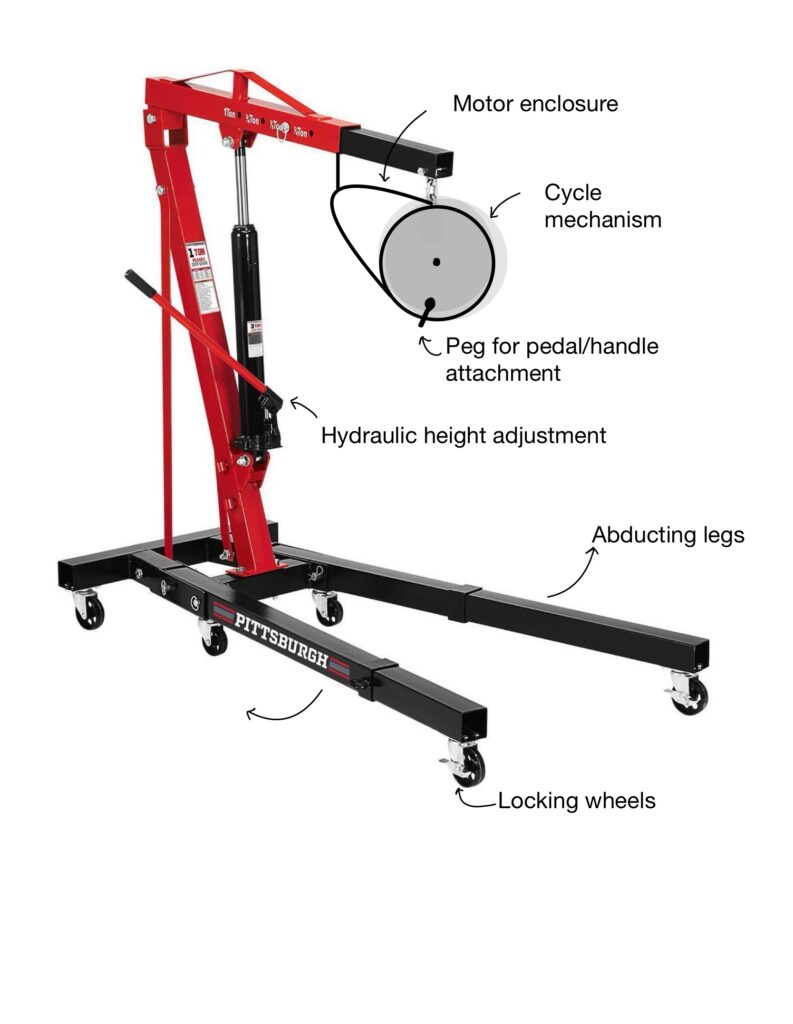
Key Design Features
| Assistive Cycling | The motorized design allows for the patient’s legs to be moved through a cycling range of motion without using their own muscle power. |
| Orthotic Boot Foot Attachment | The orthotic boot secures the patient’s foot into the device and comes in a range of sizes. It can also be inflated to provide a tighter fit. |
| Lockable Wheels | Lockable wheels allow for easy maneuverability through the ICU and for stability while in use. |
| Collapsible Design | The legs fold up and the boom folds down to decrease the footprint of the device and make storing it in a crowded ICU easier. |
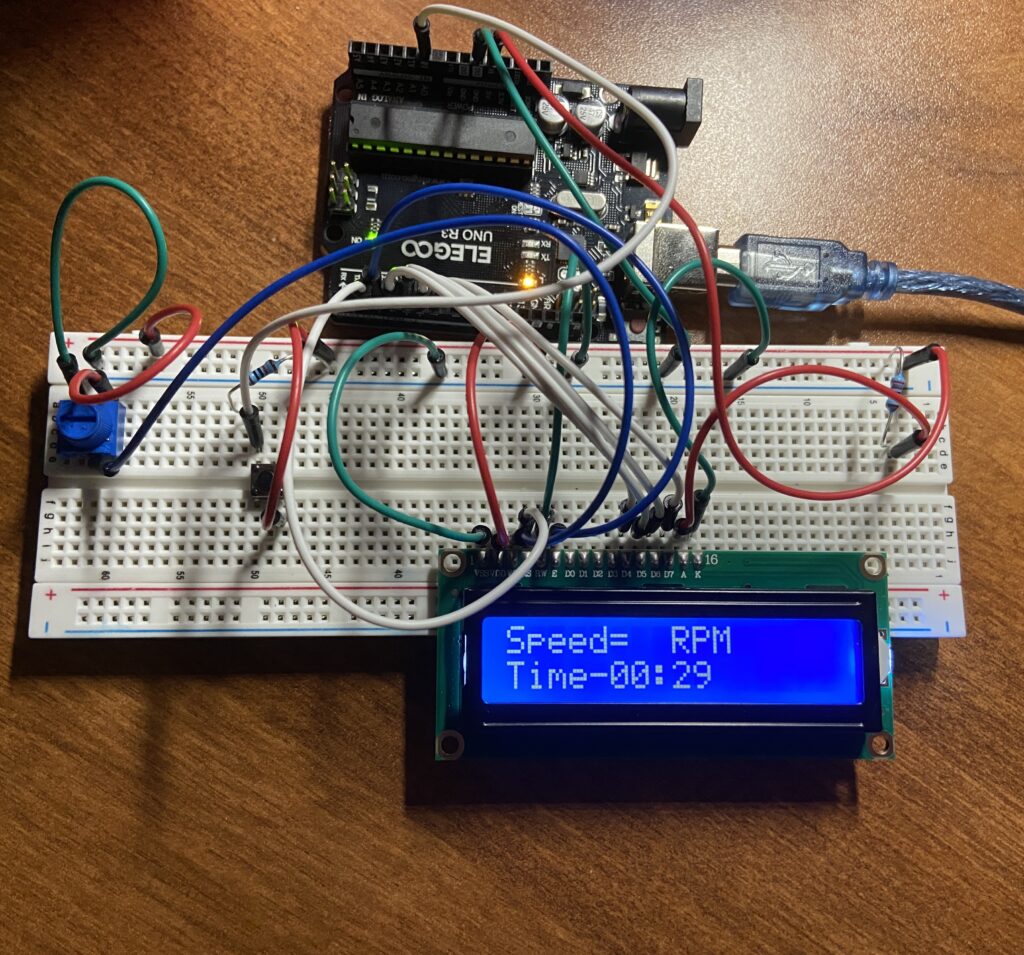
| Control Panel | The control panel allows the operator to change the direction and speed of movement and track the speed and time spent using the device. |
| Adjustable Height | The boom can be raised and lowered to adapt to various bed dimensions and patient needs and allow for easy storage. |
| 25 ft Power Cord | No need to charge batteries, the 25 ft power cord will easily plug into the many outlets in the ICU. |
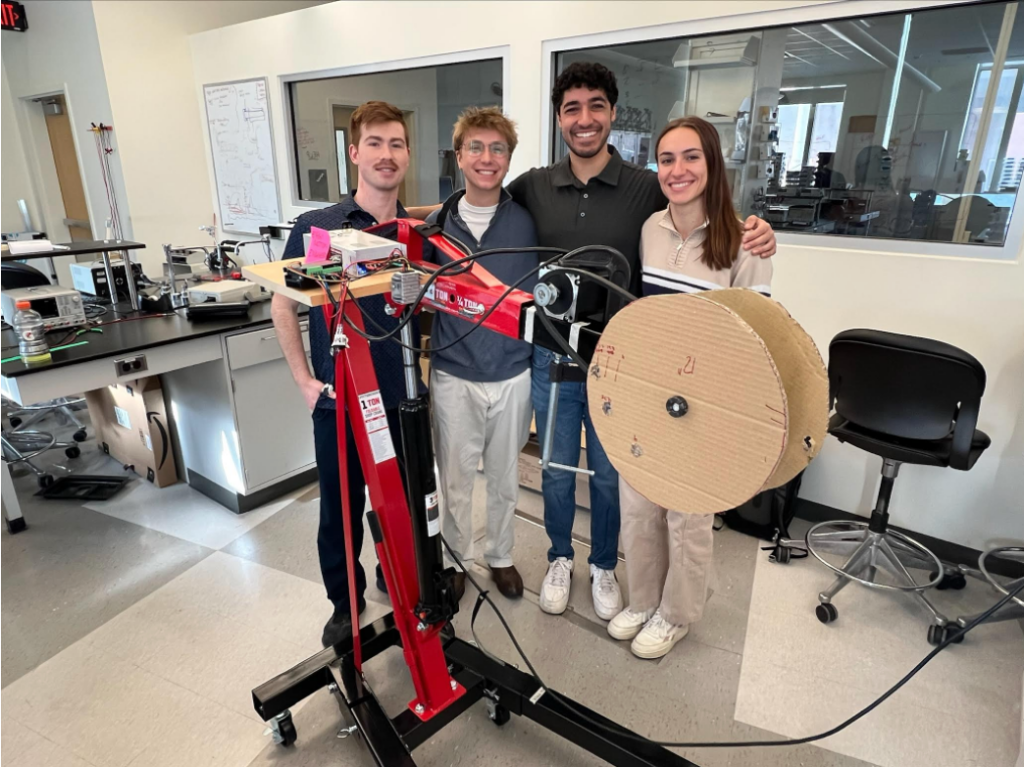
Final Prototype


Future Directions
- Enclose belts and motor
- Round edges of device
- Create lower profile foot pedals
- Enclose hydraulic lift
- Create vinyl lining for orthotic boots
Design Team
Megan Bell, Paul DeSouza, Johann Kintzel, and Matthew Tierney
Supervisor: Dr. Cherice Hill, PhD
Project Management Liaison: Amanda King
Customers

Tracy Hardes, Senior PTA, CSRS
Joseph Crumlish, DPT
Acknowledgements
We would like to acknowledge the following people for their assistance throughout the semester with this project:
Tracy Hardes, Joe Crumlish, Dr. Scott Seidman, Dr. Ben Castañeda, Dr. Cherice Hill, Jim Alkins, Samantha Kriegsman, Martin Gira, and Shawn T. Biehler
Sources
- Society of Critical Care Medicine (2024). Critical care statistics. [online] Society of Critical Care Medicine (SCCM). Available at: https://www.sccm.org/Communications/Critical-Care-Statistics.
- Schweickert, W.D., Pohlman, M.C., Pohlman, A.S., Nigos, C., Pawlik, A.J., Esbrook, C.L., Spears, L., Miller, M., Franczyk, M., Deprizio, D., Schmidt, G.A., Bowman, A., Barr, R., McCallister, K.E., Hall, J.B. and Kress, J.P. (2009). Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. The Lancet, [online] 373(9678), pp.1874–1882. doi:https://doi.org/10.1016/s0140-6736(09)60658-9.
- Takaoka, A., Utgikar, R., Rochwerg, B., Cook, D.J. and Kho, M.E. (2020). The Efficacy and Safety of In–Intensive Care Unit Leg-Cycle Ergometry in Critically Ill Adults. A Systematic Review and Meta-analysis. Annals of the American Thoracic Society, 17(10), pp.1289–1307. doi:https://doi.org/10.1513/annalsats.202001-059oc.
- Nickels, M., Aitken, L., Walsham, J., Barnett, A. and McPhail, S. (2019). 129. Critical Care Medicine, 47, p.47. doi:https://doi.org/10.1097/01.ccm.0000550886.33140.92.
- Wieske, L., Dettling-Ihnenfeldt, D.S., Verhamme, C., Nollet, F., van Schaik, I.N., Schultz, M.J., Horn, J. and van der Schaaf, M. (2015). Impact of ICU-acquired weakness on post-ICU physical functioning: a follow-up study. Critical Care, 19(1). doi:https://doi.org/10.1186/s13054-015-0937-2.
- Watanabe, S., Liu, K., Nakamura, K., Kozu, R., Horibe, T., Ishii, K., Yasumura, D., Takahashi, Y., Nanba, T., Morita, Y., Kanaya, T., Suzuki, S., Lefor, A.K., Katsukawa, H. and Kotani, T. (2022). Association between Early Mobilization in the ICU and Psychiatric Symptoms after Surviving a Critical Illness: A Multi-Center Prospective Cohort Study. Journal of Clinical Medicine, 11(9), p.2587. doi:https://doi.org/10.3390/jcm11092587.
- Patel, B.K., Pohlman, A.S., Hall, J.B. and Kress, J.P. (2014). Impact of Early Mobilization on Glycemic Control and ICU-Acquired Weakness in Critically Ill Patients Who Are Mechanically Ventilated. Chest, 146(3), pp.583–589. doi:https://doi.org/10.1378/chest.13-2046.