Abstract: Accidental disconnection of gastrostomy (G-tube) extension tubes during enteral feeding remains a clinical and caregiver challenge, impacting approximately 100,000 patients annually. Disconnections often occur during nighttime sleep, leading to missed delivery of nutrients and medications, increased caregiver burden, and heightened risk of complications. Current solutions, such as adhesive methods and belt systems, are limited by skin irritation, moisture failure, frequent replacement needs, and bulkiness, particularly for pediatric patients. An animation made by team member Ahmet Gurcan descibing the problem and the LocClip solution is shown below. The LocClip addresses these limitations through a low-profile mechanical design that locks the extension tube to the G-tube button, maintaining a secure connection without adhesives or bulky equipment. The device is simple to apply, compatible with standard extension tubes, and minimizes patient discomfort and caregiver intervention. Human factors studies and bench testing have shown that the LocClip enhances device security, reduces feeding disruptions, and provides a safer, more reliable experience. This patient-centered design has the potential to significantly improve care quality and reduce caregiver stress.

Figure 1: Render of the LocClip device by the MeDescover team.
The MeDescover team consists of 3 CMTI M.S. Student who have extensive engineering, research, development, and business experience. Each team member had over 130 hours observing various sururies in the OR through an 8 week summer rotation.
Biodesign Statement A way to prevent accidental G-tube disconnections and reduce button dislodgement in pediatric and adult enteral feeding patients, to improve reliability and reduce caregiver burden.
Gastronomy Tube Anatomy
A low-profile gastrostomy tube, commonly known as a “button,” is a medical device used to provide direct access to the stomach for feeding, hydration, or medication when oral intake is not possible. Unlike traditional long G-tubes, low-profile buttons are compact and sit flush against the skin, making them less noticeable and more comfortable for daily use, especially in active individuals or children. The device includes an external feeding port, an internal retention balloon or dome that holds it securely inside the stomach, and a one-way valve to prevent leakage.
In many modern cases, low-profile G-tubes are placed directly during the initial gastrostomy procedure, without requiring a longer tube first. The procedure involves making a small incision through the abdominal wall into the stomach, then inserting the button device. The internal balloon is deflated during placement and then inflated once inside the stomach to anchor the tube. This approach allows patients to benefit from the convenience and low profile of the button right from the start, avoiding the need for later tube replacement.
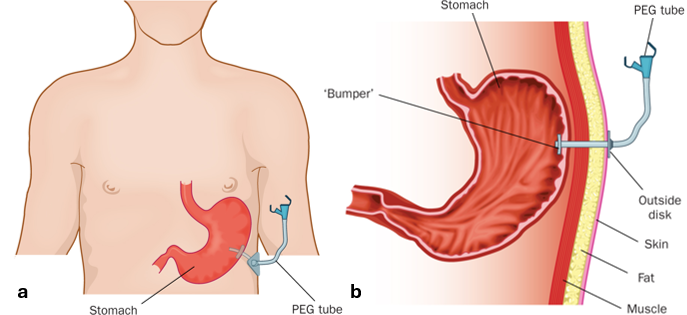
Figure 2: a) Overview of feeding tube placement in relation to the patient and b) a cross-section view of the stomach.
Low-profile gastrostomy buttons use a slot-and-key locking system to connect extension tubing during feeding, designed to ensure alignment and reduce the risk of accidental disconnection. The button has internal grooves (the “slot”), and the extension tube features a matching tab or “key” that fits into this slot. When inserted and rotated—usually 90 or 180 degrees—the extension tube is held in place as shown in Figure 3. However, despite this design, there is no true locking mechanism that physically secures the connection like a latch or clip. Instead, the system relies on friction and alignment, which means that during routine movement—especially in children or during overnight feeds—the key tab can sometimes rotate back into the open position. This can allow the extension tube to disconnect mid-feed, potentially leading to leaks, missed nutrition, or the need for caregiver intervention.
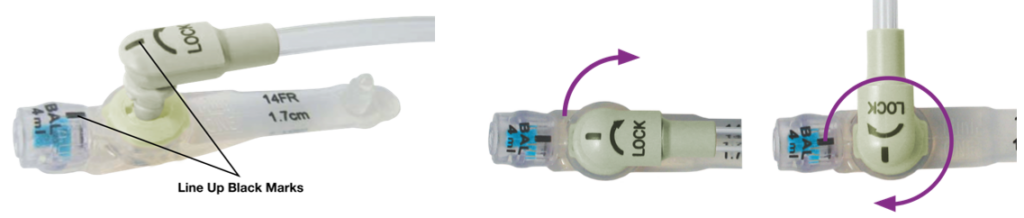
Figure 3: Process of attaching extension tube to a G-tube button.
Figure 4 shows that to prevent accidental disconnection of the extension tubing, many patients and caregivers rely on tapes or adhesive-based securement devices to hold the tube in place during feeding. These are typically applied by anchoring the extension tube to the skin or clothing to reduce tension on the slot-and-key connection. While this approach can help minimize movement, it comes with several drawbacks. Prolonged use of medical tape can cause skin irritation, redness, or even breakdown—especially around the sensitive area near the stoma. Additionally, moisture buildup at the stoma site, whether from leaks, sweat, or cleaning, often causes the adhesive to lose effectiveness. As a result, the tape may peel off or shift, requiring frequent repositioning and replacement throughout the day. This ongoing maintenance adds to caregiver burden and increases the likelihood of disconnection during routine activities.
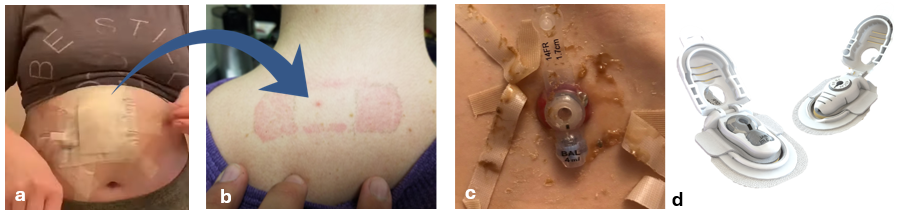
Figure 4: a) a patient adding layers of tape to keep feeding tube steady, b) allergy to adhesive c) adhesive failing in the moist environment and d) the Button Huggie, a competitor device designed to absorb messes and prevent dislodgment.
Several design concepts were considered during the development of the LocClip to address G-tube disconnection issues which are shown in Figure 5. The TubeLock was a screw-based concept that compressed the extension tube against the button to prevent disconnection. While it functioned well mechanically, its contact with feeding formula raised regulatory concerns and cleaning burdens, leading to its dismissal. The G-Patch was an early adhesive-based solution that locked the extension tubing in place while absorbing leakage, but it was rejected after feedback from users about the drawbacks of adhesives—mainly difficulty in application and skin irritation. The Mic-Lock wrapped around both the extension tubing and balloon port to block rotation, but it raised concerns due to proximity to the stoma and potential buildup of bile or formula. Patients could also remove it if they played with it, prompting an attempted fix with a TPU loop—ultimately deemed too complex. Lastly, the original LocClip evolved from these iterations, providing a non-adhesive, secure mechanical lock that prevents rotation and accidental disconnection without interfering with nutrient flow
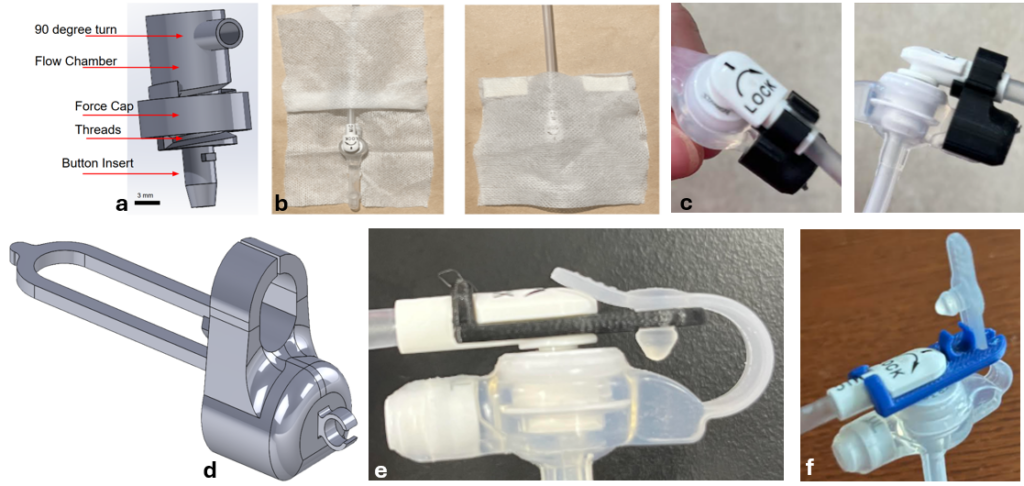
Figure 5: a) shows the 2-piece, screw-locking system of the TubeLock, b) shows the G-Patch, an absorbent, tube twist prevention system, c) the MicLock, a twist prevention system supported by the balloon inflation port, d) is the MicLock with an extension to prevent removal, e) the original LocClip where the G-tube button cork is used to prevent rotation, and f) a slotted version of the LocClip and the first incorporation of the slack clip.
The current LocClip, Figure 6, is a mechanically engineered solution designed to prevent disconnection of low-profile gastrostomy extension tubes without relying on adhesives or tape. It works by clipping over the G-tube button and the extension set in a way that physically blocks rotation of the key tab, ensuring the connection stays locked during feeding. Unlike earlier concepts, it does not come into contact with formula flow paths, which helps minimize regulatory complications and simplifies cleaning. The device is easy to apply, reusable (upto 2 weeks), and intentionally kept separate from the stoma site to avoid skin irritation or interference with wound healing. Its design provides a reliable and caregiver-friendly way to reduce accidental dislodgement, nighttime feeding interruptions, and the need for constant supervision.
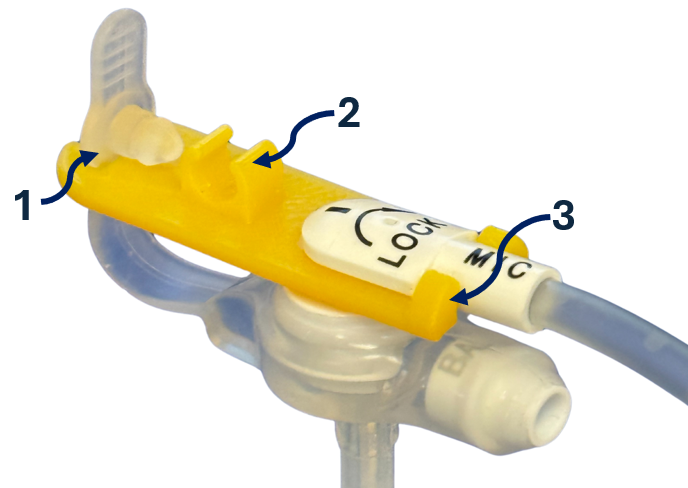
Figure 6: The patent pending version of the LocClip is designed to have the body extend to prevent the G-tube tab from sticking up and to decrease amount of rotation allowed. The arms going over the extension tube were decreased to save on material cost. The arms were also stiffened to prevent device removal and increase durability.
To ensure the LocClip effectively prevents unintended rotation of the extension tube, a mechanical verification test was performed to assess whether the G-tube tab could be rotated to the unlocked position under normal use. The test showed that while the tube could be physically rotated with 1.7–2.3 lbs of applied force, typical forces from patient movement, such as turning during sleep, remained under 0.5 lbs. Additionally, applying 0.5 lbs of force only rotated the tube ~50 degrees, as shown in Figure 7 —well below the 180 degrees needed for disconnection—demonstrating that accidental unlocking is unlikely during daily use.
The SlacClip feature underwent force disengagement testing to confirm its ability to act as a breakaway mechanism that protects against G-tube dislodgement. This component was designed to fail below 14 lbs of force, with an ideal breakaway force near 10 lbs to add a safety buffer. Results showed that vertical pulls averaged 4.3 lbs and horizontal pulls averaged 3.5 lbs, staying safely below dislodgement thresholds while still allowing caregivers to loop tubing through it without excessive difficulty.
Further testing addressed the device’s tamper-evident design. The LocClip is engineered so that it cannot be removed without visible breakage, acting as an immediate visual indicator of tampering. This was validated through mechanical stress tests that ensured any removal would result in permanent deformation, giving clinicians a reliable way to detect unauthorized removal.
In addition to mechanical safety, impedance modeling and flow testing were conducted to ensure the LocClip does not interfere with enteral nutrition delivery. A fluid dynamics analysis in COMSOL was performed to model how the device geometry might affect formula flow. Using flow impedance equations and approximations for formula viscosity and tube dimensions, it was shown that the LocClip’s design introduces negligible resistance compared to baseline extension sets. Experimental validation involved flowing formula through both looped and unlooped setups, showing no measurable difference in flow rate or pressure buildup. This confirmed that the device preserves feeding performance and does not cause occlusion or delay during use.
Finally, to ensure pediatric safety, the LocClip was tested against U.S. Consumer Product Safety Commission (CPSC) standards for small parts. The device was made longer than the allowable choking dimensions and tested for resistance to age-appropriate manipulation forces. These changes ensured compliance with pediatric safety standards, making it more resistant to swallowing and tampering by children.
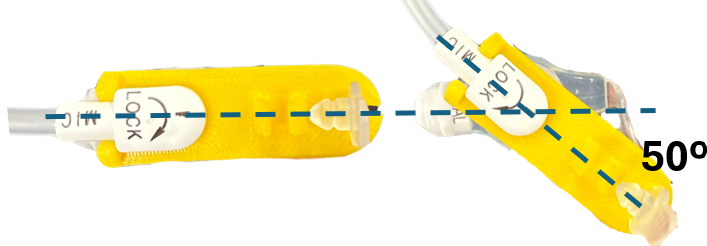
Figure 7: Maximum rotation the LocClip allows, preventing the extension tubing from moving to an unlocked position.
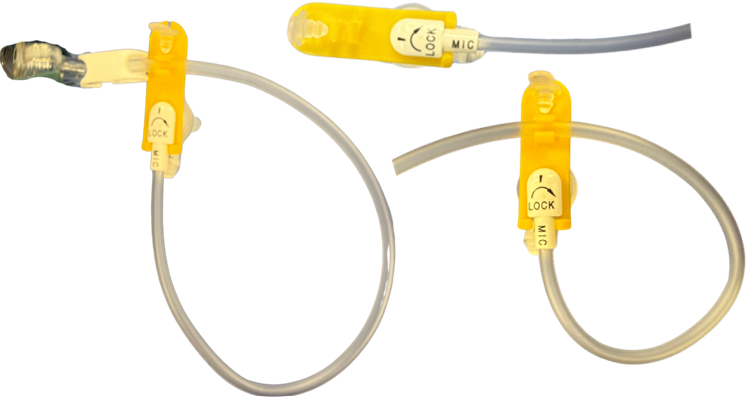
Figure 8: The maximum impedance by the Slack Clip is 5% of the occlusion rate of most standard pumps.
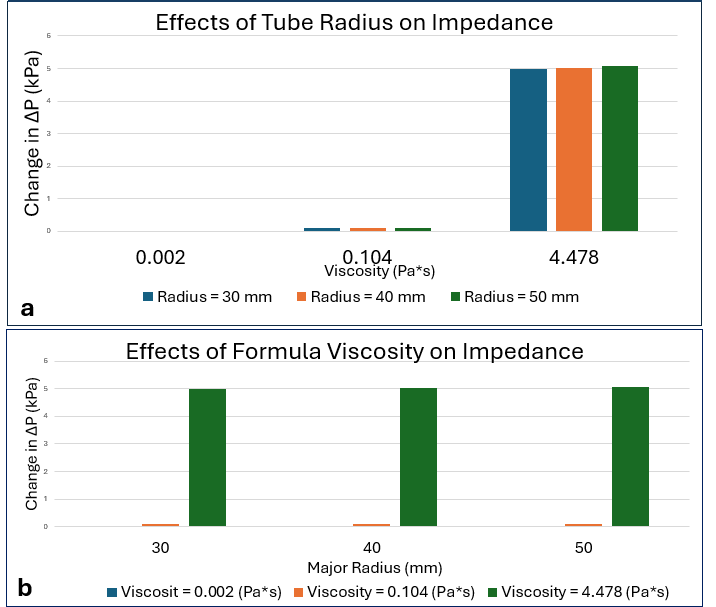
Figure 9: The maximum impedance by the Slack Clip is 5% of the occlusion rate of most standard pumps.
Conclusion The LocClip is a tamper-proof device which prevents accidental disconnections of extension tubing from feeding button without impeding nutrient flow.
Acknowledgements: We thank CMTI academic directors Dr. Greg Gdowski, Dr. Amy Lerner, and Dr. Jonathan Stone, as well as all our CMTI instructors for teaching us critical skills in engineering, regulatory affairs, intellectual property, biology, communication, and validation. We also want to thank the BME Senior Engineer Martin Gira. We are grateful to Dr. Nicole Wilson and Dr. Derek Wakeman from URMC Department of Pediatric Surgery for their guidance and support, and to Bailey Garlipp (URMC) for providing feeding supplies for our testing. We also thank patients and families who participated in interviews and provided valuable insight into their daily challenges.

