Team
Abdalrahman Almallahi
Timmarie Gallagher
Maysoon Harunani
Phuong Le
Rosemary MacLean
Ellie Richard
Project Supervisor
Regine Choe, Ph.D.
Customer
Nicole Wilson, Ph.D, M.D.
Paul Kupicha
Background Information
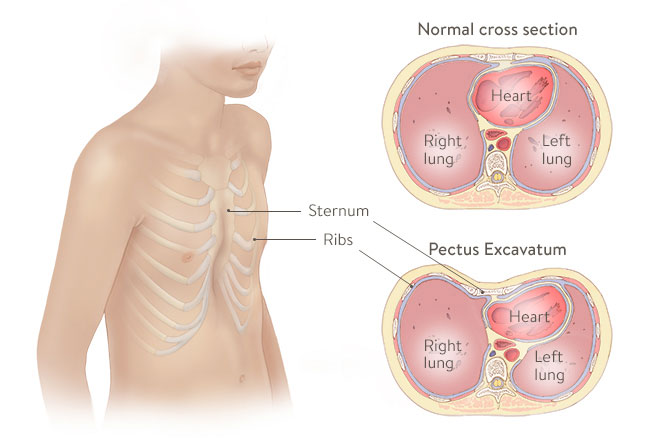
Medical Condition
Pectus excavatum (PE) is the most common chest wall abnormality, making up about 87-90% of cases.1 The abnormality is characterized by a depression in the chest, specifically the sternum and surrounding costal cartilages. This depression of the chest can cause health problems associated with the compression of the heart and lungs.2 Compression of the heart can lead to decreased cardiac output, mitral valve prolapse, and arrhythmia. The complications involving the pulmonary system include restrictive lung disease, pulmonary atelectasis, paradoxical respiration, and more frequent and prolonged respiratory infections.1
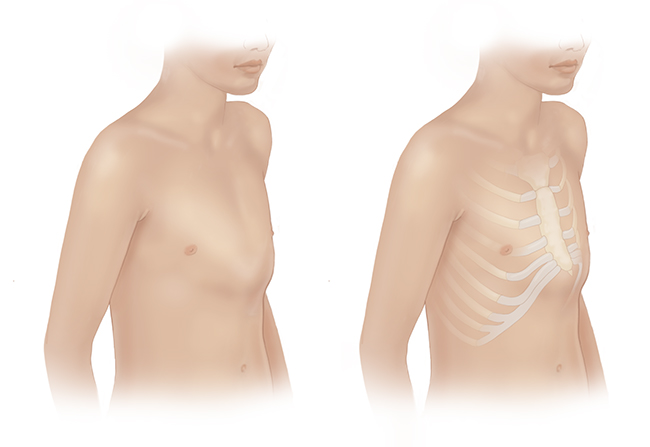
The second most common chest wall abnormality is pectus carinatum (PC), which accounts for about 5% of chest wall abnormalities.1 PC is characterized by the outward protrusion of the sternum or rib cage. It is generally not as dangerous physiologically as PE and often does not present other symptoms. In the cases where there are symptoms, potential ones are tenderness at the protruded region and reduced pulmonary endurance.3
PE and PC can also have a psychological impact on patients such as withdrawal from social activities, a high degree of body image dissatisfaction, and low self-esteem. This leads to an overall decrease in quality of life in addition to the possible physical health issues.4
Scanning
3D optical scanning has recently been proposed for application in research settings as an alternative to computed tomography (CT) scans for quantifying chest wall abnormalities. This would aid in reducing the exposure to radiation and allows for more frequently scanning to evaluate and monitor the progression of treatment.7 Dr. Wilson and Paul Kupicha proposed designing a scanning apparatus to improve the research in this field and increase patient compliance by showing their progression in treatment more frequently in a quantifiable way.
Problem Statement
The current methodology for 3D optical scanning at the Golisano Children’s Hospital Center for Chest wall Reconstruction is not able to repeatedly produce standardizable scans due to its manual process of holding the scanner and walking around the patient. The Optical Scanning for Chest wall Abnormalities (OSCA) project is focused on designing a system to produce more standardized and reliable 3D images for analyzing the progression of chest wall abnormality treatment over time.
Scenario
The scanning device will aid in the acquisition of chest wall scans that are used during the treatment process for PE and PC. Dr. Nicole Wilson and her team are currently manually scanning their patients, using an iPad and the Structure Mark II sensor. The scanner is held one meter away from the patient’s chest and level with their chest wall. The handheld scanner is then moved around the patient, trying to follow a circular path while keeping the iPad and scanner level.
The new scanning apparatus will be adjusted according to the height of the patient and the user will push the scanning vertical arm along the guided circular path around the patient. The user will stop and pause for incremental scanning as prompted by the system’s built-in stops. This allows for consistency in the positioning of the iPad and rotation for each keyframe, both of which aid with producing precise and reproducible scans.
Major Design Requirements
- Full 360˚ rotation around patient
- Produce accurate measurements from 3D scan
- Accommodate a wide height range
- Support the weight of the patient
- Entire system fits in the exam room
- Device can be sanitized between patients
- System can fit in the storage space
- The system can be efficiently transported
- The system can be efficiently assembled
Earlier Prototypes
Concept Prototypes
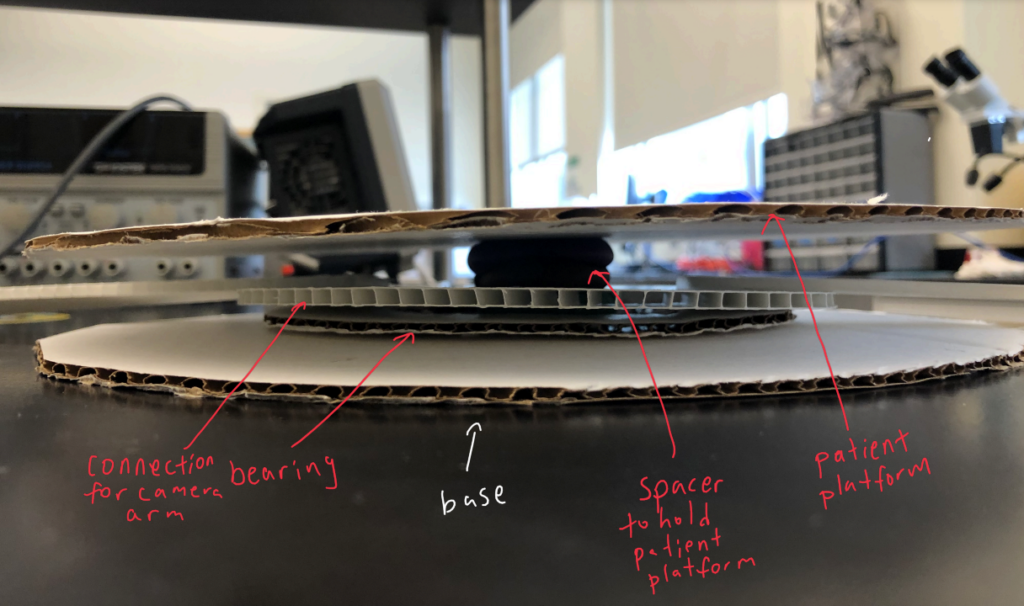
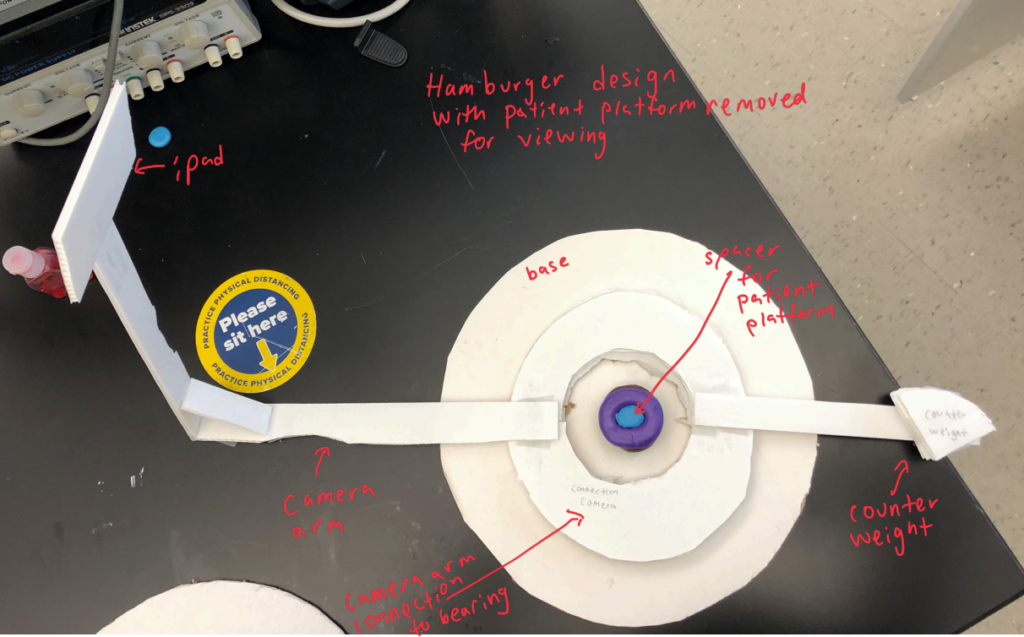
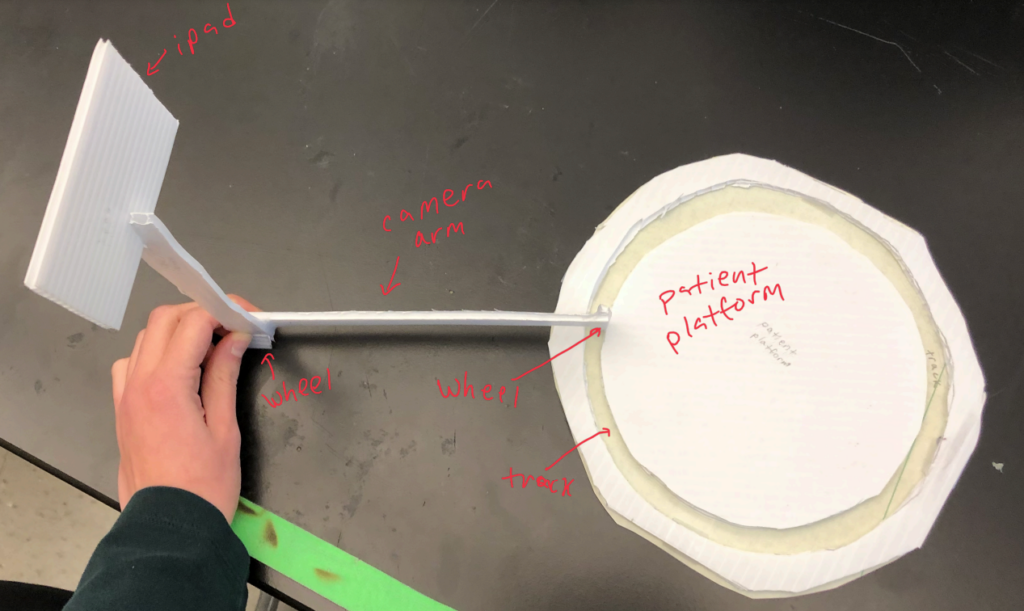
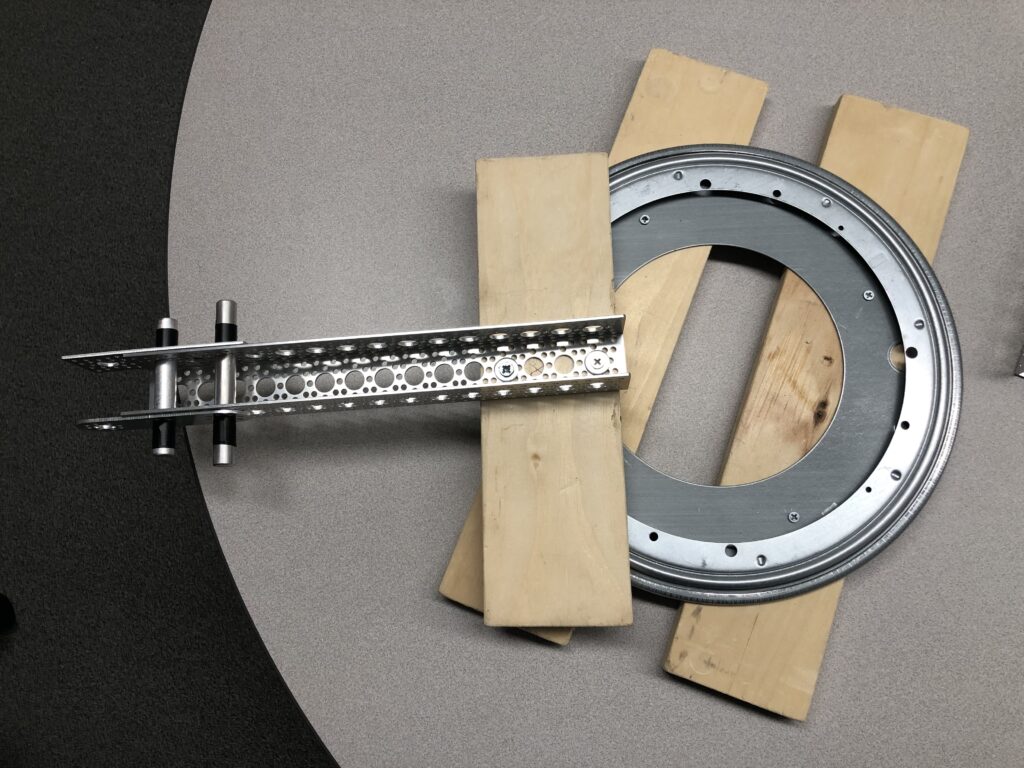
We made two cardboard models to help visualize our ideas. The first design involved the use of a lazy susan bearing to rotate an arm with the scanner attached. The second design consisted of rotating the arm by having a wheel that moved along a track around the platform that the patient would stand on. These models brought up questions about what the track would be made of, the design of the wheel designs, and the availability of circular tracks. With these considerations, we decided to move forward with the lazy susan design.
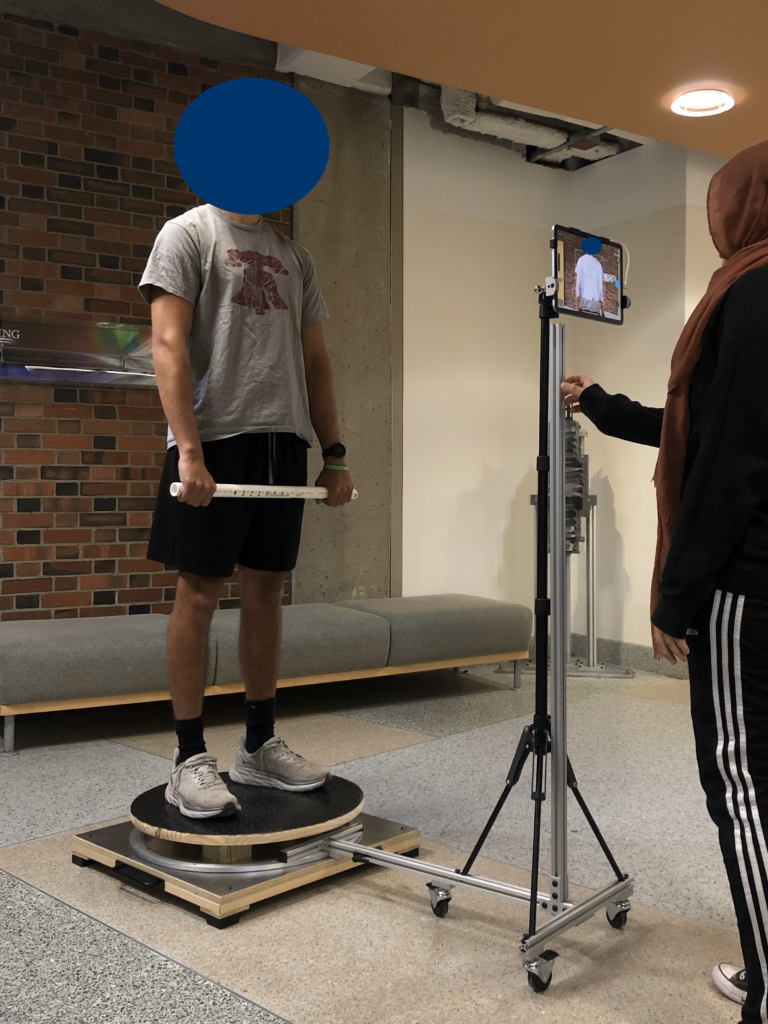
Our next step in the prototyping process was to create a larger-scale prototype with more realistic materials. In this prototype, we used a lazy Susan bearing with eight stops built into it. We chose this bearing because it allows the ‘key frames’ feature of the scanner to create the three-dimensional image. This prototype was made up of wood and aluminum U-beams. The wood was used to help hold the bearing in place and manipulate it while the U-beam acted as the rotating horizontal arm which would theoretically have the vertical arm and scanner attached to it. The model confirmed the functionality of the lazy Susan design.
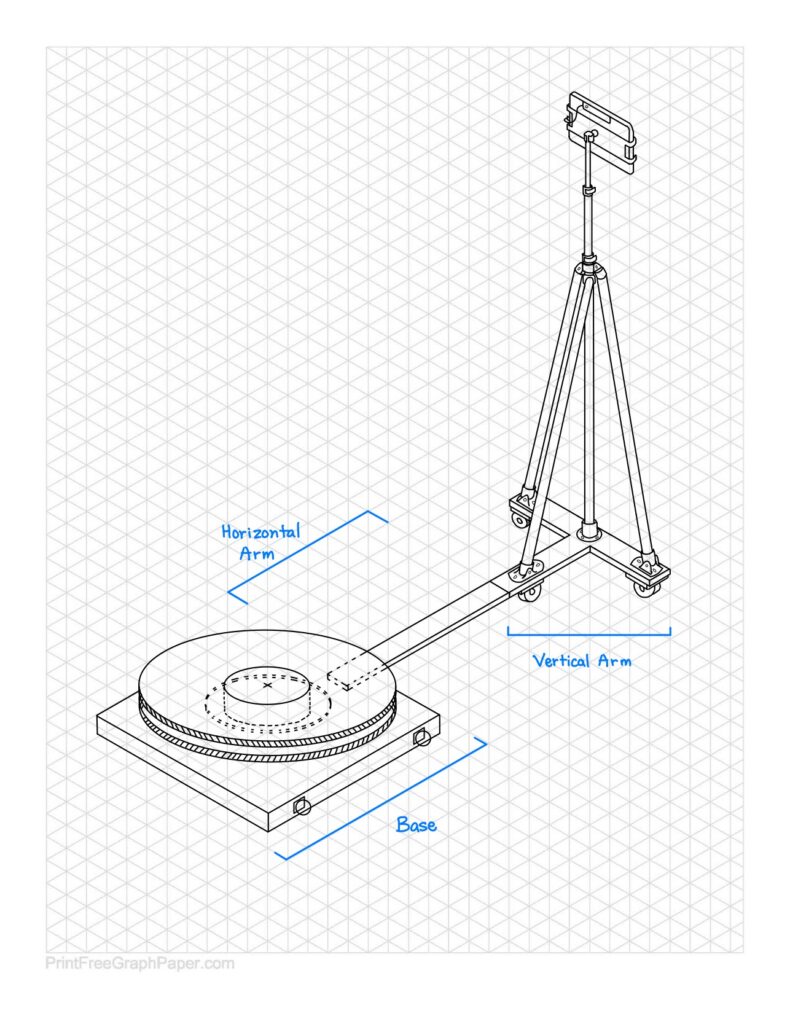
Sketches and CAD Model
In addition to physical prototypes, we made sketches by hand and designed a 3D model of our prototype using Fusion360. Below is a sketch and 3D model of an earlier prototype involving the use of telescopic tubing and flanges for the vertical arm.
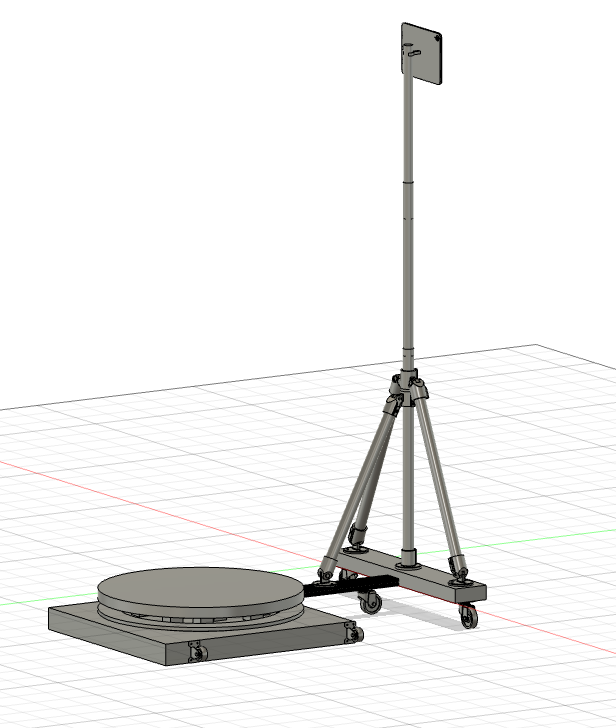
Final Prototype
The final prototype can be divided into two subsystems, the base and the vertical arm with a horizontal arm connecting the two. The base consists of a patient platform held up by supporting pillars. The platform in which the patient stands on has a plastic-textured top to allow for a cleanable non-slip surface. This patient platform is encircled by a lazy Susan bearing which has the horizontal arm attached and allows for 360 degree rotation about the patient. Attached to the horizontal arm is the vertical arm which is made up of a tripod with an iPad attachment clamped to the top of it. The tripod has telescoping poles allowing for fine adjustment of the height of the scanner. Three wheels are attached to the vertical arm base and horizontal arm to allow for the system to be rolled smoothly around the patient and to the storage room. The vertical arm also includes a metal handle placed next to the tripod that can be pushed to move the scanner around the patient. The horizontal arm has a break that allows for the base and the vertical arm subsystems to be separated for easy transportation and storage. The base can be tipped onto attached wheels and the user can grip a handle and roll it away.
Future Directions
To further enhance the success of the OSCA design, various future directions could be considered:
- Improve the lazy susan’s stopping mechanism to provide a more secure grip on each detent
- To better align with clinical sanitization requirements the wooden components could be substituted with plastic or metal materials
- Incorporate a measuring tape attachment to record the scanner’s height, which could be useful for research purposes
- Improve the base handle to ensure easy transportability of the product for individuals of varying heights. This could involve exploring several options such as telescopic or retractable prototypes, that allow for different height configurations.
- Add a more permanent weight to the vertical arm to reduce torque
Acknowledgements
We would like to dedicate special thanks to Dr. Nicole Wilson for bringing forth the idea as a senior design project. We are also very grateful to Marty Gira for his help during the fabrication process, and our supervisor, Dr. Regine Choe, for providing guidance throughout the OSCA project since day one. Finally, we would like to thank Dr. Scott Seidman for his tremendous support and mentorship in this senior design course.
References
- Goretsky, M. J., Kelly, R. E., Jr, Croitoru, D., & Nuss, D. (2004). Chest wall anomalies: pectus excavatum and pectus carinatum. Adolescent medicine clinics, 15(3), 455–471. https://doi.org/10.1016/j.admecli.2004.06.002
- Sharma, G., & Carter, Y. M. (2022). Pectus Excavatum. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK430918/
- McHam, B., & Winkler, L. (2022). Pectus Carinatum. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK541121/
- Steinmann, C., Krille, S., Mueller, A., Weber, P., Reingruber, B., & Martin, A. (2011). Pectus excavatum and pectus carinatum patients suffer from lower quality of life and impaired body image: a control group comparison of psychological characteristics prior to surgical correction. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery, 40(5), 1138–1145. https://doi.org/10.1016/j.ejcts.2011.02.019
- Pectus Excavatum. (n.d.). Stanford Medicine Children’s Health. Retrieved from https://www.stanfordchildrens.org/en/service/chest-wall/pectus-excavatum.
- Pectus Carinatum. (n.d.). Stanford Medicine Children’s Health. Retrieved from https://www.stanfordchildrens.org/en/service/chest-wall/pectus-carinatum.
- 3D Modeling and Printing. New Technology Committee. (2022). In PedSurg Resource https://www.pedsurglibrary.com/apsa/view/PedSurgResource/1884013/all/New_Technology_Committee