Introduction
The photodynamic therapy system utilizes an optical probe that consists of nine individual optical fibers each with a 200 μm core diameter and 0.22 numerical (Bridger et. al, 2021). The probe, manufactured by Pioneer Optics Company, is used to measure diffuse reflectance properties of deep-tissue abscesses and deliver the appropriate light dose needed to activate a photoactivated drug used in killing abscess bacteria. Through our project, we aim to develop an appropriate calibration system for the probe so that when it is inserted into the abscess cavity it is calibrated to a standard that will allow the measurements to accurately model abscess reflectance properties.
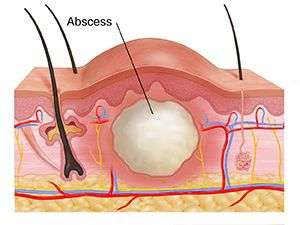
An abscess is a fibrous capsule filled with pus that forms as a result of the immune response to a bacterial/fungal infection within the human body (Bridger et al, 2021). White cells collect and combine with damaged tissue and germs in the infection site, creating pus. The collagen fibers of surrounding dying tissue form a pseudocapsule encapsulating the pus and preventing the infection from contacting the rest of the body. The usual treatment of abscesses involves surgical drainage of this purulent fluid and the use of antibiotics systematically to kill the remaining bacteria. However, because surgical draining doesn’t fully remove all fluid in the abscess, the biofilm of bacteria on the walls of the abscess has a chance to become resistant to antibiotics if not fully killed. Because of this, the abscess can reoccur as bacteria that weren’t fully killed rebreed within the warm isolating environment of the abscess, leading to low cure rates in some patients (Bridger et al, 2021).
Due to the lack of effectiveness of antibiotics on resistant bacteria, photodynamic therapy was introduced as an alternative to current surgical practices for treating abscesses. The treatment of interest utilizes photoactivated drugs to kill bacteria instead of using antibiotics. It works to kill microbial cells by the excitation of a photosensitizer or non-toxic dye with low-intensity visible light of the appropriate wavelength producing reactive oxygen species within the abscess (Kharkwal et al., 2011). Since radical oxygen species are toxic to bacteria, this technology kills bacteria more thoroughly and solves the issue of dealing with antibiotic-resistant bacteria. With PDT for deep-tissue abscesses, the optical properties of each individual patient’s abscess vary as a result of its size, shape, location, composition, etc. Thus, it’s necessary to predetermine optical properties such as reflectance and absorbance for each individual abscess so that treatment can be normalized to deliver a patient-specific light dose to activate the photosensitizer to kill bacteria. Since our project aims to develop a calibration device that will mount to this probe, the opening of the calibration port must fit the dimensions of the probe and hold it securely in place while blocking out as much extra room light.
References:
Bridger, K. G., Roccabruna, J. R., & Baran, T. M. (2021). Optical property recovery with spatially-resolved diffuse reflectance at short source-detector separations using a compact fiber-optic probe. Biomedical Optics Express, 12(12), 7388. https://doi.org/10.1364/boe.443332
Kharkwal, G. B., Sharma, S. K., Huang, Y.-Y., Dai, T., & Hamblin, M. R. (2011). Photodynamic therapy for infections: Clinical applications. Lasers in Surgery and Medicine, 43(7), 755–767. https://doi.org/10.1002/lsm.21080
