Introduction
Prostate cancer is ranked the second most commonly diagnosed cancers among men worldwide, while being named the fifth most common cancer deaths. Robot assisted radical prostatectomy (RARP) exists as the gold standard to treat localized prostate cancer, which entails surgical removal of the prostate gland, seminal vesicles, and part of the vas deferens with the assistance of a da Vinci robot. A major risk of prostate removal surgery is loss of erectile function and incontinence post-operation.
Our team is developing an enhanced prostatectomy training simulator to support the refinement of surgical technique and reduce patient risk during robot-assisted radical prostatectomy (RARP). Building on an existing surgical phantom, our focus is on simulating anatomically accurate neurovascular bundles (NVBs) that provide real-time feedback on tissue damage during practice procedures. Through a combination of sub-system testing, prototype validation, and user-informed metrics, we aim to establish a proof-of-concept for our damage detection system and guide future development efforts.
Problem Statement
We seek to de-risk robot-assisted radical prostatectomy (RARP) surgeries by building upon an existing surgical training model, allowing surgeons to practice procedures, refine nerve sparing techniques, and increase surgical confidence before operating on patients.
To achieve this, our team built anatomically faithful neurovascular bundles (NVBs) and a damage detection system closely simulate operative conditions and offer continuous feedback on NVB damage.
Customer Scenario
Our device is specifically designed for practicing RARP surgeons and for the purpose of being used during training and educational sessions. The current setup entails:
- Operative room equipped with a da Vinci surgical system
- Surgery will be performed under camera guidance.
- Surgical arms are used to move, cut, or cauterize the PVA hydrogel prostate model .
- Real-time footage of the operation will be recorded for educational use post-op.
- Device placed on operating table, mimicking placement of a patient during surgery
- Continuous data from our device’s damage detection system will be collected and analyzed for additional educational purposes after surgery is complete.
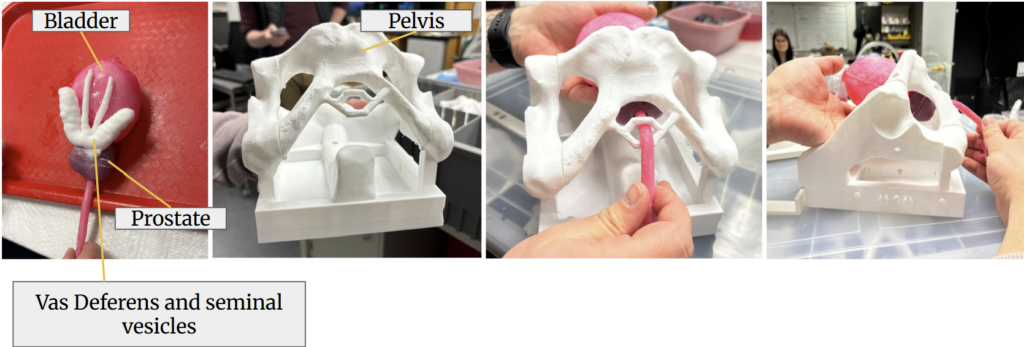
The surgical phantom in the SURGE lab consists of the bladder, prostate, and surrounding organs in a pelvic cavity.
- 3D printed elastic resin model of pelvic floor
- PVA model of the prostate, bladder, seminal vesicles, vas deferens, and urethra
PVA periprostatic fat - Cotton batting
- Grounding pad
- Conductive rubber stretch cords colored with silicone-based paint
Design Concept
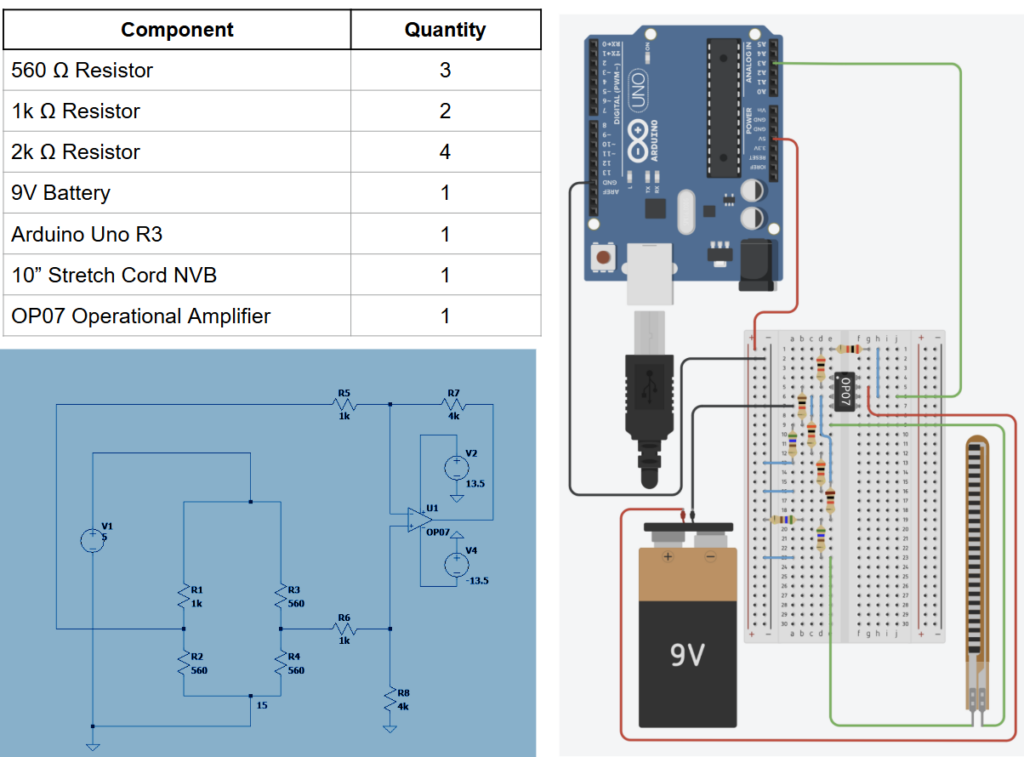
As you contact the NVB, the resistance of the cord changes. This proves especially useful for us: when implementing the NVB in a circuit, resistance changes in the NVB can be read out as voltage changes, which allows us to use electrical sensing as a means for detecting tissue damage. Different types of contact produce different electrical signals, which can be time-correlated with the da Vinci camera footage to provide insight into how different types of surgical techniques damage the NVBs
Below is our hardware circuit design.
Prototyping & Feedback
After shadowing a practice RARP and in consultation with Dr. Tom Oshinski at the SURGE lab, we simulated various types of damage in vitro, or with an isolated set of the prostate and NVBs. We applied the following types of damage:
- Environmental disturbance (e.g. bladder/prostate moves)
- Direct contact with NVB (e.g. forceps touch)
- Digging or stretching of NVB
- Nicking (e.g. partial severance)
- Full severance of NVB
From these data, we determined the difference thresholds that corresponded to various types of damage. Through iterative prototyping we adjusted the gain of the circuit to adjust the signal to noise ratio, or distinguish between significant NVB contact and environmental noise. Continuous feedback between testing and prototyping informed our final model. We displayed this in the form of a MATLAB graphical user interface (GUI).
Future Directions
Given more time, we would have liked to test alternative conductive materials to improve consistency, sensitivity, anatomical realism in tactile feedback along with visual accuracy in coloration. Our current NVBs are made of rubber stretch cord and painted over with a fleshy, pink color; while this was sufficient for our customer’s first model, real NVBs exist in a web-like structure. These materials would preferably be some type of conductive polymer or biomaterial compatible with the polymers present in the current SURGE lab model. Exploring these materials would enhance the realism of the surgical phantom and minimize the gap between training and real-world applications.
We would also like to look into streamlining the calibration for voltage data collection. The baseline voltage between NVB samples vary; this is likely due to material properties, manufacturing inconsistencies, slight variations in probing length, and differences in stretch cord tension. These inconsistencies affect the thresholding values used for damage detection and require calibration for each NVB. Future improvements refine post-processing to efficiently establish a consistent 0V baseline for each NVB.
Meet the Team Behind It All
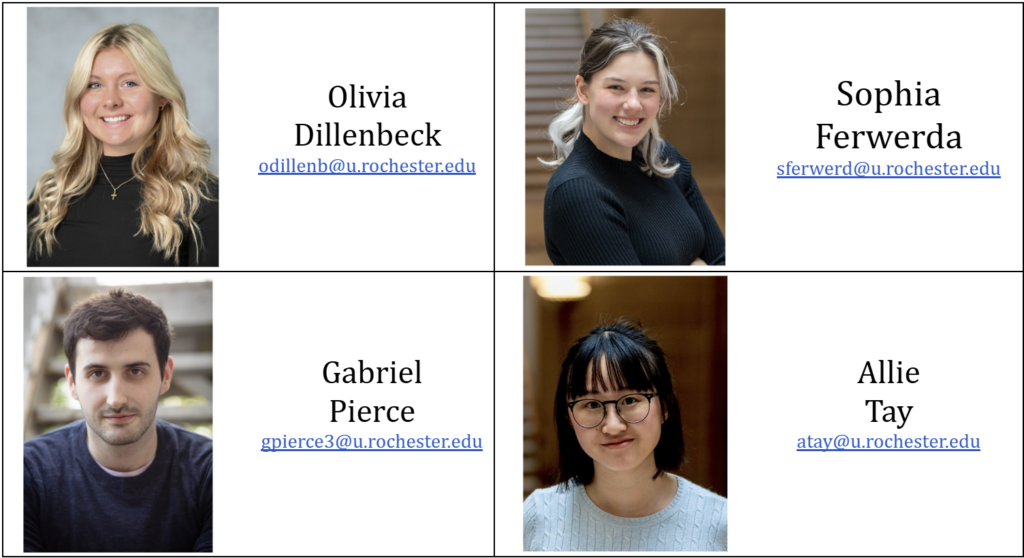
Hey there! We’re Olivia Dillenbeck, Sophia Ferwerda, Gabriel Pierce, and Allie Tay — a group of biomedical engineering students specializing in Cell & Tissue Engineering and Biomechanics.

Together, we bring a well-rounded mix of skills to the table (and lab bench). From polymer molding to hydrogel fabrication to building tiny houses, our team has strong hands-on experience with biomaterials and DIY-ing. We’ve also served as teaching assistants for introductory circuits, where we supported students in building physical circuits, explaining foundational theory, and using simulation tools. Beyond the technical side, we bring a range of communication experience — including research, theatre performance, and journalism. We value not only the science behind our work, but how we share it.
Feel free to reach out to us!
Our Customer
Our customer is Mitchell Hoestermann, M.S. at the SURGE lab, a surgical simulation lab that develops anatomical models for urology surgeries.
Our Supervisor
Our supervisor is Dr. Marisol Herrera-Perez.

