Archive of BME Design Day Projects
This page lists projects, by year, from Biomedical Engineering (BME) undergraduates in their senior year, and CMTI MS students. You can also view online galleries of our projects on the Hajim Senior Design website.
| 2024 2019 2016 2013 2010 2007 | 2023 2018 2015 2012 2009 2006 | 2022 2017 2014 2011 2008 2005 |
Class of 2024
Senior Projects
- Neonatal Endotracheal Placement Probe – A novel method for ETT insertion.
TEAM: Hannah Bushey, Liz McGinn, Laura Nafis, Benedikt Winzer, Thomas Xue
Customer: Gal Barbut, M.D., Department of Pediatrics, Neonatology, UR Medical Center
Supervisor: Edward Brown, Ph.D., Biomedical Engineering, Neuroscience, James Wilmot Cancer Center, University of Rochester - The At-Home Fertility Testing Device – A device that can measure the fertility hormones for each user.
TEAM: Aashee Budhwani, Mansi Kothari, Victoria Millette, Ava Saffren, Julia Wallace
Customer: Meg Mendelson, MiCare Path
Supervisor: Kanika Vats, Biomedical Engineering, University of Rochester - Bladder Fullness Detector – Wearable electrode device to detect fullness for use in monitoring geriatric patients in hospitals.
TEAM: Nick Dente, Kate Issac, Lam Nguyen, Fiorella Rivadeneira, Bella Smith
Customer: Donald Gibson, Tom Kennedy, Dan MacDonald Garrett Mattimore, Curbell Medical Products, Inc.
Supervisor: Veena Ganeshan Ph.D., Biomedical Engineering, University of Rochester - Microscope Pluck and Dispense System – An artificial intelligence toolbox to retrieve and relocate cells in microbubble arrays.
TEAM: Severin Ilhnat, Aubrey Lantham, Arthur Masiukiewicz
Customer: Lisa DeLouise, Ph.D., M.P.D, Dermatology, Biomedical Engineering, Electrical and Computer Engineering, UR Medical Center and University of Rochester, Keith Bozek, First Consulting Inc.
Supervisor: Whasil Lee, Ph.D, Biomedical Engineering, Pharmacology and Physiology, University of Rochester - Cardiac Phantom Model for Left Atrial Appendage Occlusion Procedures – A modular heart model with physiological tissue characteristics, capable of blood flow facsimile and evaluation of left atrial appendage occlusion procedures.
TEAM: Kevin Gery, Aasim Hawa, Tochukwu Iyke-Nzeocha, Seth Schlosser, Wendy Zimmerman
Customer: Tim Adolf, Benjamin Boseck, Matthew DeClerck, Sandra Madanat, Simbi Maphosa, John Moyer, LSI Solutions
Supervisor: James McGrath Ph.D., Biomedical Engineering, University of Rochester - The Pneumoneers – To develop a device that utilizes cutting-edge technology to improve the precision and safety of realtime lung visualization during bronchoscopy procedures.
TEAM: Aeden Angelone, Arlo Gow, Delainey Hebble, Christian Voloshen
Customer: Jonathan Thomson, Medtronic
Supervisor: Steve McAleavey, Ph.D., Department Chair, Biomedical Engineering, Electrical and Computer Engineering, Rochester Center for Biomedical Ultrasound, University of Rochester - Testing Osia Bone Conduction – A device to evaluate the conduction of vibration through bone in the operating room.
TEAM: Mariam Bamba, Cassidy Christie, Vedat Duzgezen, Diana Karosas, Audrey Yu
Customer: Benjamin Crane, M.D., Ph.D., Department of Otolaryngology, UR Medical Center
Supervisor: Regine Choe, Ph.D., Biomedical Engineering, Electrical and Computer Engineering,University of Rochester - Combined Surgical Driver – Design and develop a combined motorized and static screwdriver with variable chuck and power mechanisms.
TEAM: Ian Bergquam, Marissa Bortel, Robert Constantine, Joshua Leadem, Caroline Murnane
Customer: Dave DiStefano, M.D., Department of Orthopaedics, UR Medical Center
Supervisor: Greg Gdowski, Ph.D., Biomedical Engineering, Center for Medical Technology and Innovation, University of Rochester - Tick Collection– A device to collect ticks in Costa Rica for further study.
TEAM: Lawrence Chen, Rachelle Gomez-Guevara, Sarah Manning, Anjali Patel
Customer: Timothy Dye, Ph.D., Department of Public Health Sciences, Department of Obstetrics and Gynecology, UR Medical Center
Supervisor: Anne Luebke, Ph.D., Biomedical Engineering, Neuroscience, University of Rochester - Lens Benders – Engineering a non-invasive way to measure stress and deformation in contact lens.
TEAM: Noah Freedman, Sakura Herron, Kendall Kohout, Regan Merkin
Customer: Michael Clark, Alex Kotelsky, Ph.D., Terra Spurgeon, Bausch + Lomb
Supervisor: Mark Buckley, Ph.D., Biomedical Engineering, Center for Musculoskeletal Research, Center for Visual Science, University of Rochester - Prostate Biopsy Phantom – Creating reusable training equipment for Prostate Biopsies to improve sampling and reduce patient risk.
TEAM: Loralai Crawford, Hunter Gilbreath, Julissa Morales
Customer: Tom Osinski, Mitchell Hoestermann, Department of Urology (SMD) SURGE Lab, UR Medical Center
Supervisor: Richard Waugh, Ph.D., Biomedical Engineering, University of Rochester - Pulseless Pulse Oximetry – A device to measure blood oxygen saturation in pulseless patients.
TEAM: Hanna Costa Carvalho, Joel DeVries, Daniel Kelly, Aliza Klein, Sikhulile Vilane
Customer: Mark Marinescu, M.D., Department of Cardiology, UR Medical Center
Supervisor: Edmund Lalor, Ph.D., Biomedical Engineering, Neuroscience, University of Rochester
CMTI MS Student Projects
SplashGuard
TEAM: Duy Doan, Ben Amadi, Miguel Yakouma
Biodesign statement: A way to perform off-pump LVAD implant to prevent blood splash and eliminate risk of thrombosis for end-stage heart failure patients.DuraMate by NeuroTech Innovations
TEAM: Aveisha Maharaj, Kaveri Salunke, Vincent Mu
Biodesign statement: A way to perform off-pump LVAD implant to prevent blood splash and eliminate risk of thrombosis for end-stage heart failure patients.LapFlex-PDT: Novel Delivery Device for Background Perforated Appendicitis (PA)1,2,3 Photodynamic Therapy
TEAM: Mitchell Kershner, Phuong Le, and Korry Wirth
Biodesign statement: Develop a laparoscopic light-emitting device to optimally deliver photodynamic therapy (PDT) in the abdomen to reduce the bacterial load in patients with perforated appendicitis (PA).Sherpa Pro – ORIF Precision Drill Guide Device
TEAM: Garrett Dietrich, Ben Hulbert
Biodesign statement: To design a system that simplifies the process of drilling pilot holes and ensures proper alignment of locking screws in ORIF procedures.IllumiCath, by W.E.L.D.
TEAM: Judy Monickaraj, Jazmin Phommavanh, Aveisha Maharaj, Ignacio Rodriguez
Biodesign statement: An instrument for GYN surgeons that minimizes bladder injury in vaginal hysterectomy patients to avoid urinary complications and bladder repair procedures during the anterior colpotomy.
( back to top)
Class of 2023
- BME Photos from Design Day 2023 (4/28/23)
- 2023 BME Program (pdf)
- 2023 Video: Dean Heinzelman Welcome
- BME Student Project Gallery
- CMTI MS Student Project Gallery
Senior Projects
- Workload Stress Analysis Device- A System for the Analysis of Workload Stress in the Pediatric ICU
TEAM: Ibrahim Adelwahab, Douglas Allen, Eunate Alzaga, Ignacio RodriguezCustomer: Adam Christopher Dziorny, M.D., Ph.D., Physician Scientist, University of Rochester Medical Center
Supervisor: Edmund Lalor, Ph.D., Biomedical Engineering, Neuroscience, University of Rochester - CelluCov- A COVID lateral flow assay antigen test that can degrade in a non-toxic manner in soil or ground sewage water lines while still maintaining low cost per unit and high sensitivity levels.
TEAM: Katherine Broun, Duy Doan, Judy Monickaraj, Claudia Garcia, Miguel Yakouma
Customer: Jeffrey W. Beard, Ph.D., Dermatology, University of Rochester Medical Center
Supervisor:Richard Waugh, Ph.D., Biomedical Engineering, University of Rochester - Photodynamic Therapy Calibration Device- A device that allows for accurate and repeatable calibration of an optical probe that will be used in Photodynamic Therapy (PDT) for the treatment of abscesses in a hospice setting.
TEAM: Riya Shah, Zaynab Dantsoho, Dinesh Sangadi
Customer: Timothy Baran, Ph.D., Imaging Sciences, Optics, University of Rochester Medical Center
Supervisor: Michael Giacomelli, Ph.D., Biomedical Engineering, Optics, University of Rochester Medical Center - Hemiblock Spacer- A means and tool to acquire improved access to posterior spaces for cement removal
TEAM: Joshua Rainbolt, Faisal Reza, Natnael Ayalew, Edward Niles, Nathan Gehris
Customer: Thomas G. Meyers, M.D., M.P.T., Orthopaedic Surgery, University of Rochester Medical Center
Supervisor: Marisol Herrera-Perez, Ph.D., Biomedical Engineering, University of Rochester Testing Osia Bone Conduction Efficacy (TOBE) System- a quantitative method of evaluating the impact of a skull plate on bone conduction.
TEAM: Cassidy Christie, Audrey Yu, Vedat Duzgezen, Diana Karosas, Mariam Bamba
Customer: Benjamin Crane, M.D., Ph.D., Department of Otolaryngology, UR Medical Center
Supervisor: Regine Choe, Ph.D., Biomedical Engineering, Electrical and Computer Engineering, University of RochesterImproved Innate Light Avoidance Shuttle Box- An imrpoved appartus able to present various forms of visual stimuli to a mouse, record the mouse’s resulting behavior, and analyze the changes in behavior.
TEAM: Karina Bridger, Aparajeeta Majumder, Christopher Lu, Sameer Jain
Customer: Michael Telias, Ph.D., Opthalmology, Neuroscience, University of Rochester Medical Center
Supervisor: Laurel Carney, Ph.D., Biomedical Engineering, University of Rochester- Obstacle Visulization For Wheelchair Users
TEAM: Eli Lawrence, Kevin Lee, Diana Alcedo de Obarrio, Vahni Tagirisa, Victoria Warner
Customer: Matthew Oliveri Optical Scanning for Chest wall Abnormalities (OSCA)- designing a system to produce more standardized and reliable 3D images for analyzing the progression of chest wall abnormality treatment over time.
TEAM: Abdalrahman Almallahi, Timmarie Gallagher, Maysoon Harunani, Phuong Le, Rosemary MacLean, Ellie Richard
Customer: Nicole A. Wilson, Ph.D., M.D., Biomedical Engineering, Pediatrics, Pediatric Surgery, University of Rochester Medical Center
Supervisor: Regine Choe, Ph.D., Biomedical Engineering, Electrical and Computer Engineering, University of RochesterSurgical Loupe Improvement- Creating an attachment for dentists and surgeons to change the declination angle and improve posture during long hours of operations.
TEAM: Alyssa Hoogs, Katia Teta Iliza, Andrew Moglianesi, Claude Nzabandora
Customer: Sarah Neimanis, M.D., Plastic Surgery, Golissano Children's Hospital
Supervisor: Edward Brown, Ph.D., Biomedical Engineering, Neuroscience, James Wilmot Cancer Center, University of RochesterTissue Surrogate For Anastomoses- Partnering with LSI Solutions to create a demonstration model for surgeons in training to simulate the closure process of these anastomoses under various pressures and pulsatile flows.
TEAM: Leah Badger, Matt Cosentino, Baoqi Max Liu, Kelsey Stites, Xiang Tang
Customer: Benjamin Boseck & Carrie Carhill, LSI Solutions
Supervisor: Amy Lerner, Ph.D., Biomedical EngineeringUpper Extremity Instrument for Testing Shoulder Mobility- Providing a quick and effective method of evaluating key movements performed in everyday life so that patient care can be improved.
TEAM: Garret Dietrich, Abbey Kampel, Mitchell Kershner, Lesley Leatherman, Carissa Minarovich, James Norberg
Customer: Ram Haddas, M.D., Orthapaedics, Center for Muscloskeletal Research, University of Rochester.
Supervisor: Mark Buckley, Ph.D., Biomedical Engineering, Center for Musculoskeletal Research, Center for Visual Science, University of Rochester
CMTI MS Student Projects
Class of 2022
Senior Projects
- APIJECT NEEDLE
TEAM: Abdullah Abuomar, Chloe Jones, Hana Kalco, Katelin Klaric, Ronald Lakony, Helen Shammas
Customer: ApiJect Systems - Automated Histology- Automating the mounting process in microtome histology
TEAM: Amanda Adams, Ahmet Gurcan, Connor Heckman, Gradi Bamfonga, Ruyi (Lauren) Li
Customer: Walter Richard Burack, M.D., Ph.D., Pathology and Laboratory Medicine, Cancer Center, University of Rochester Medical Center
Supervisor: James McGrath Ph.D., Biomedical Engineering, University of Rochester - BAXTER SMART ROOM- Designing a prototype to address smart infusion pump related problems that harm the patient experience in hospitals
TEAM: Thu (Tracy) Le, Nejat Can, Ngoc Tram Nguyen, Oishee Rahman
Customer: Karen Fellows, Baxter International
Supervisor:Amy Lerner, Ph.D., Biomedical Engineering - CERVICAL SPINE DIARY- Aiming to build better habits in the user that improve their posture over time and prevent neck pain from poor posture, through data collection device.
TEAM: Ahmad Abdal Qader, Anapaula Avila, Hamza Hasan, Luis Borja
Customer: Ramzi El Hassan, M.D., M.S., Department of Physical Medicine & Rehabilitation
Supervisor: Laurel Carney, Ph.D., Biomedical Engineering, University of Rochester - CT-GUIDED ANGLE DEVICE- A device made to stabilize needle entry and advancement at set angles during CT-guided procedures.
TEAM: Arpeet Dabhade, Linh Hoang, Tracey Moyston, Jacob Roccabruna
Customer: Akm A. Rahman, M.D., D.O., Ph.D., Department of Imaging Sciences (SMD), University of Rochester Medical Center
Supervisor: Regine Choe, Ph.D., Biomedical Engineering, Electrical and Computer Engineering, University of Rochester - HIP BROACHING SYSTEM- A device intended to collect data on impaction force and rotational movements during the broaching process in total hip arthroplasty
TEAM: Stuart Aldred, Anurag Dwivedi, Kate Lindsey, Zachary Muench, Reshul Narhari
Customer: John Gerald Ginnetti, M.D., Department of Orthopaedics (SMD)
Supervisor: Whasil Lee, Ph.D., Biomedical Engineering, Pharmacology and Physiology, University of Rochester - FALL PREVENTION- Creating a comfortable and non-intrusive device to measure bladder impedance, and reduce patient falls
TEAM: Benjamin Gwinnell, Megan Hauer, Chloe Li, Danielle Marouni, Parinitha Sharma
Customer: Curbell Medical
Supervisor: Veena Ganeshan Ph.D., Biomedical Engineering, University of Rochester - JUNGLECUP SURVEILLANCE- a small, portable, and weather-proof device that can operate in Costa Rican environments that attracts and traps mosquitoes to determine the prevalence of dengue virus
TEAM: Ava Giorgianni, Jacob Kelley, Tiana Salomon, Kaelyn Schloss, Caroline Stockwell
Customer: Tim Dye, M.D., Medical Anthropology, Universeity of Rochester Medical Center
Supervisor: Edward Brown, Ph.D., Biomedical Engineering, Neuroscience, James Wilmot Cancer Center, University of Rochester - LESS SCARY CAST REMOVAL- Creating a system and device that can remove casts in a way that is less scary for kids.
TEAM: Anna Baber, Thomas Dolan, Melisanda Feliz, Abbey Gilman, Delaney Martino
Customer: Natasha O'Malley, M.D., Orthapedics, University of Rochester Medical Center
Supervisor: Mark Buckley, Ph.D., Biomedical Engineering, Center for Musculoskeletal Research, Center for Visual Science, University of Rochester - NEONATAL CPAP ADAPTOR- An improved neonatal CPAP mask that reduces the amount of pressure exerted on the neonate’s delicate skin and detects air leakage at the mask-neonateinterface.
TEAM: Justin Jablonski, Wendy Jung, Befikadu Mekonnen, John Moyer, Ivana Pacar, Terra Spurgeon
Customer: Andrew Dylag, M.D., Biomedical Engineering, Pediatrics-Neonatology.
Supervisor: Anne Luebke, Ph.D., Biomedical Engineering, Neuroscience, University of Rochester - NERVE CONDUCTION- Implementing the design of an intraoperative nerve monitoring system that detects and prevents damage to the upper extremity’s peripheral nerves.
TEAM: Meah Ahmed, Carolyn Kochek, Lindsey Rudtner, Priscila Passerotti Vaciski B
Customer: Jonathan Stone, M.D., Biomedical Engineering, Neurosurgery, Neuorology, University of Rochester Medical Center
Supervisor: Dr. Ross Maddox, Ph.D., Biomedical Engineering, Neuroscience, University of Rochester Medical Center - COMMODE FOR NEUROGENIC BOWEL- Improving the quality of life of individuals suffering from neurogenic bowel.
TEAM: John Bates, Chastity Chavez, Madison Lang, Alexander Rivera, Camila Ruiz Vega
Customer: Sara Salim, M.D., Physical Medicine & Rehabilitation, Medicine, Geriatrics/Aging, University of Rochester Medicine.
Supervisor: Richard Waugh, Ph.D., Biomedical Engineering, University of Rochester - VASCULAR ACCESS SAFEGUARD- Incorporating an antiseptic component to protect the needleless connector of all vascular access lines, reducing the risks and associated costs of central line bloodstream infections (CLABSI).
TEAM: Marianna Aviles Jubis, Ingrid Dukundane, Hannah Glucksman, Mimi Jung
Customer: Kathleen Pratt, PICC-Team Line Insertion Nurse, URMC
Supervisor: Michael Giacomelli, Ph.D., Biomedical Engineering, Optics, University of Rochester Medical Center
CMTI MS Student Projects
- SAFE MEDICAL MONITORING SYSTEMS- DetectIV
TEAM: Theo Couderc, Sophie Mackenzie, Rebecca Mathurin
Biodesign Statement: A device for anesthesiologists to detect unwanted infiltration and extravasation from delivery of intravenous fluids to reduce incidence of effects such as pain, swelling and risk of necrosis during the intraoperative period. - MITRAL VALVE PAPILLARY RING
TEAM: Ejiroghene Davies-Okarevu, Katarina Lichak
Biodesign Statement: A device for cardiothoracic surgeons to use to retract the leaflets of the mitral valve to increase visualization of and access to the sub–valvular structures during mitral valve repair surgery. - STMEDICAL
TEAM: Hadi Wehbe, Lucas Lassinger, Stephen Wells
Biodesign Statement: A device aiming to reduce complications during surgery by preventing Organ Punctures, Trocar movments and poor tissue alignments during wound closure. - BUBBLE TROUBLE
Team: Michael Lee, Samuel Maquet
Biodesign Statement: A medical device that aims to eliminate bubbles in all surgical procedures to aid healthcare professionals prepare contrast agents faster, safer and simpler. - CALCATCH
TEAM: Nandita Bhowmik, Bahie Ezzat
Biodesign Statement: A device for cardiothoracic surgeons to capture embolic debris from falling into the left ventricle during surgical aortic valve replacements (SAVR) to reduce the number of particulates left behind and mitigate their associated risk of stroke. - LEMICI PATIENT CAMERA
TEAM: Warish Orko, Mark Truskinovsky
Biodesign Statment: A remotely operated camera to increase the accessibility of wound healing teleconsultations. - SCREWIT KIT
TEAM: Allison Coon, Abbi Miller, Sylvia Zhong
Biodesign Statement: Reducing unfavorable fixation outcomes suffered by patients during ORIF surgeries due to incorrect screw placement
Class of 2019
2019 BME Photo Gallery on FacebookSeniors
Sinus Inspectors
Robert Crews, Amanda Hornick, Penelope Subervi, Alaa Bukhari, Lucy Franzen
A device that accurately indicates the probability that patients of different ages, sexes, and craniofacial anatomies have sinusitis in a way that is easily interpretable by primary care physicians or other medical professionals during an office visit. This device is a safer pre-screening method for sinusitis than CT scans, as it exposes patients to a negligible amount of ionizing radiation.

Bladder Monitor
Ahmed Selmi, Camila Garcia Wright, Kharimat Lora Alatise, Alyssa Gardiner
The overall goal for the Bladder Monitor Device team is to design a wearable device that will measure the fullness of the bladder and notify a nurse or caretaker when the bladder is reaching full capacity. This will be done by measuring the bioimpedance of the bladder. The purpose of this device is to decrease the amount of falls that take place due to people attempting to use the bathroom unassisted or bed wetting that also may occur. This device will be designed to be used in long term care facilities, post-surgical care, and by any person whose locomotion is hindered in any way.
Finger Stick: Reliable Finger Stick Blood Samples
Brett Tingley, Xiaoyi (Louisa) Cao, Dilshawn Gamage, John Fernando
Create a device that can collect fingerstick capillary blood samples in a less variable manner so that capillary blood can be used for accurate point-of-care diagnostics.
Field Blood Testing (KERJ Biologics)
Kavi Shankar, Erik Patak, John Lisi, Rebecca Moffat
Field medical providers such as paramedics have to make many care decisions with limited information beyond subjective physical symptoms. The application of field blood diagnostic testing would give providers a greater ability to properly care for patients.The introduction of a portable, point of care blood potassium measurement device would allow diagnosis of hyperkalemia suspicions with more confidence and overall improve the quality and thoroughness of care given to patients. We aim to develop a point of care potassium test that can work with a small blood sample obtained via an IV catheter for use in field triage decisions.
EchoMount Team
William MacCuaig, Shafieul Alam, Dominique James, Tiffany Nicholas
Our device is a mounting system that will hold an ultrasound transducer to monitor for blood clots after reconstructive surgery.
Infant Carrying Device Team
Samantha Myers, Haein Son, Rachael Pletz, Aisha Rivera
An infant carrying system which allows a parent with accessibility concerns to safely transport their child while using a walker.
Kidney Dialysis
Connor Virgile, Seung Hyun Kim, Victor Zhang
The Kidney Dialysis Interface Team is working with Fengyi Jiang (customer) from Fresenius Medical Care under the supervision of Dr. Dean Johnson (supervisor). Our project aims to develop a bench-top interface device that automatically monitors solution flowing in an experiment to test new dialyzers and other dialysis products. The device will be part of a larger project to create a simulated patient testing model for researchers to evaluate new technologies.
Ligament Tensioning
Aaron Lowin, Ryan Aspenleiter, Chang Gui, Sonam Topgyal, William DeMaria
The primary objective of this project is to design a novel tensioning device that measures and holds a desired tension on an ACL graft during reconstructive surgery in order to improve patient outcomes (e.g., reduced pain, reduced recovery period, no need for second intervention) and reduce the complexity and invasiveness of the current method.
Medical Pump Fluid Team
Molly Ferris, Collin Richards, Joe Carrier, Miles Markey
Bacterial buildup within catheters and IV lines are a significant problem due to the easy transport of this bacteria into a patient’s bloodstream. 250,000 to 400,000 individuals are diagnosed with bloodstream infections related to catheters each year costing between $300 million and $2.3 billion per year in medical expenses. The purpose of our project is to develop a disposable IV fluid sensor that detects presence of biofilms in IV lines in conjunction with Baxter’s Infusion Pump System. Our device implements stainless steel electrodes that emit changing resistance as biofilms collect on their surface. The goal of our final prototype is to demonstrate that it is feasible to measure biofilm presence in an IV line while maintaining fluid flow rate and patient safety.
THOR Designs Workforce Accessibility
Rebekah Abrams, Hannah Goldring, Olivia Uttamsingh, Taryn Milnes
THOR Designs, with aid from our supervisor Dr. Mark Buckley, is working with a local company in Rochester called Unistel to improve one of their assembly lines. Unistel is proud to employ people with a variety of disabilities, and the team that we are working with at Unistel produces dust caps for military and first responder radios made by Harris Corporation. Ryan Ortiz from Unistel has tasked THOR Designs with increasing the accessibility and efficiency of their dust cap assembly line while minimizing costs.
Project C-Collar
Emma Luke, Aleena Jamal, Nancy Bansbach, Anna Olsen
Cervical collars are designed to immobilize and stabilize the axial skeleton during suspected spinal injury; however, the current design lacks these functions. The goal of Project C-Collar is to design a new cervical immobilization device that effectively splints the axial skeleton and is accessible to all medical healthcare providers, both in the field and in a hospital setting. The collar will ideally be quick to apply, easy to store in an ambulance or hospital, imaging compatible, adjustable to a variety of sizes, and low in cost.
Nerve Phantom
Maura McCartney, Jamie King, Frances McAfee, Nick Drogo, Richard Simcic
A nerve block is a procedure using imaging to locate problematic nerves and administer a block to treat the pain. The sympathetic stellate ganglion is difficult to image using ultrasound due to the similar density of the surrounding tissue and depth within the body. The proposed idea is to utilize the natural emitted signal from the stellate ganglion for more accurate needle placement. Current nerve phantoms do not have electrophysiological properties needed for this proposed idea. Therefore, we will develop an electrophysiologically accurate phantom to be used by medical residents in the hospital to learn and practice this new technique.
AV Fistula
Jiajin (Lincoln) Zhao, Manikanta Nori, Conor Shanahan, Kimberly Richards
Patients with end-stage renal disease require a kidney transplant or dialysis treatment. The arteriovenous fistula (AVF) has become the preferred method for vascular access because of its effectiveness in increasing blood flow via a surgical connection between an artery and vein in the forearm. Sonavex has created EchoMark and EchoSure, to aid in detecting early post-operative blood flow complications in patients. Our team has created a benchtop phantom to mimic physiologic flow for an AVF. The model will simulate high-velocity, pulsatile flow patterns at various levels of post-operative conditions for the AVF’s maturation process using materials and flow rates physiologically similar to those found in patients.
Pitch Perfect Solutions
Abril Aguirre, Gabriel Guisado, Chantelle Lim, Nathaniel Silvia
Our team was tasked with designing a pre-sized implant that can be easily customized during surgery and a depth gauge that allows depth measurement from varying angles and provides better visualization of medialization depth through the laryngoplasty window in the thyroid cartilage. This new design will improve the precision of this surgery by minimizing surgical time, mitigating suboptimally-shaped implant, which will ultimately improve the patient’s voice and surgical outcome.
OCM Colposcopy
Victoria Breza, Abby Williamson, Grace Weyand, Yue Qi
Colposcopy procedures are used during the cervical cancer screening process. Our hope is to improve the sensitivity and specificity of a colposcopy procedure while reducing the potential cervical damage by integrating optical coherence microscopy (OCM) into a contact probe that can perform an optical biopsy of regions of interest on the cervix.

Center for Medical Technology & Innovation (graduate students)
IASO Surgical Solutions
Ariana Cervantes, Devon Foggio, Alyssa Marzella
OMOS is a surgical table accessory utilized in anterior cervical spine surgeries. OMOS provides a surgeon sterile control of patient positioning throughout procedures allowing for increased visualization on x-ray images and decreased risk to the patient.

Hemonamic
Huy Nguyen, Emily Grey, Elana Chazen
The hemonamic is a flow control device that provides dynamic regulation of blood flow to various parts of the body to reduce lower limb complications of patients on extracorporeal membrane oxygenation (ECMO).
Envisient
Brenna Schnell, Anli Lin, Halie Hotchkiss
Our device addresses a way to clear obstruction of the surgical field during endoscopic sinus surgery in order to improve visualization and reduce intraoperative time.
BIG Cardiovascular
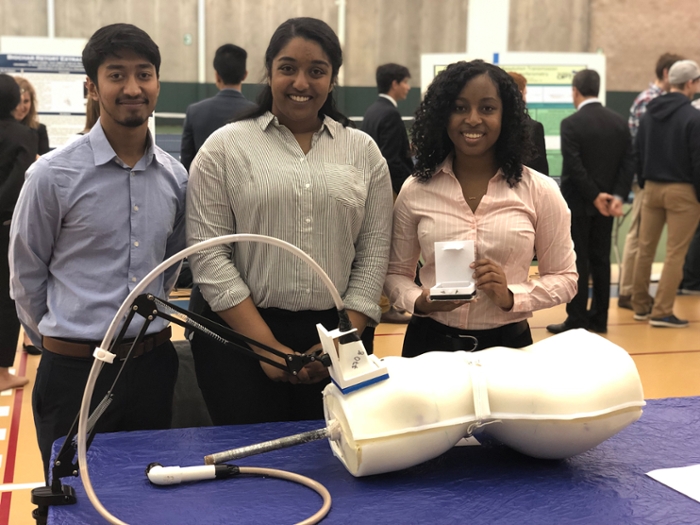
Gavin Hambrose, Rebecca Macaluso, Ivy Mannoh
A way to stabilize the post-operative bisected sternum in delayed closure cases to allow safe and successful patient movement while supporting cardiac recovery during open chest management.
Go-Flex
Jane Fong, Kwasi Nimako, April Tsang
The GoFlex technology will promote dynamic dorsiflexion assistance and support of foot drop patients. In addition, the device will provide data analytic information to the user to show patient progress over a period of time visually.
Anoptix
Veronica Valencerina, Christian Keenan, Jennifer Fukagawa
Anoptix is developing a system to continuously monitor external mechanical compressions to the eyes and orbits during prone-positioned surgeries. This device will notify the anesthesia provider of adverse pressures in order to elicit actions to alleviate these pressures and therefore decrease the likelihood of post-operative vision loss, a temporary or permanent loss of sight after prone-positioned surgeries.

( back to top)
Class of 2018
2018 BME Photo Gallery on FacebookSeniors
Guiding US IV
Kwasi Nimako, Veronica Valencerina, Kate Bushway, Anisha Khosla
A device to aid in the Ultrasound IV insertion process in an emergency room setting.
C-Arm X-Ray Improvements in the OR
Harshita Narang, Emily Grey, Shuang (Grace) Chang, Chi Huang
Improved C-Arm X-Ray machines for neurosurgeries.

Plasma Separation Team
Xuan (Monica) Sun, Mollie (Eva) Hansen, MaryAnne Achieng, Huy Nguyen
Designing a system to separate plasma from whole blood patient samples in less time than centrifugation for Ortho Clinical Diagnostics.
OR Communication
Jake Krapf, Anna Hrbac, Anyah Wright, Christian Keenan
A device or system that will be used to aid surgeons with various hearing abilities communicate while operating on patients.
The ThighCyclers
Erik Backstrom, Iain Wright, Kelly Tighe, Kyle Ruffner
An accessory device for adaptive cycles to promote safer, more comfortable rides for individuals with leg weakness due to stroke, TBI or other medical conditions.

Advancement of Breast Pump Accessibility
Helen Yang, Katelyn Offerdahl, Renee Brigham, Rachel Larkin
Working towards improving access to breastfeeding education and resources for mothers of infants in the neonatal intensive care unit.
TubercALERT!
Ramel Morales, Andrew Hollomon, Corrine Kennedy, Sam Kann
To monitor areas at high risk of spreading tuberculosis bacteria, our device detects the concentration of airborne tuberculosis, thus indicating locations where attention should be directed.
Moh's Surgery Teaching Tool
Jason Kim, Mackenzie Harris, Ryan Bowen
A device for dermatology residents to practice planning facial skin reconstructions.
Wheelchair Improvements
Zijie (James) Sha, Hye Mi (Abby) Kim, Harrah Newman, Alexandra Wolkoff, Michael Zhang
Creating a mechanism to enable wheelchair users improved ability to access their belongings. 
Saccadic Adaptation
Nicholas Boldt, Sang Park, Emily Palacio, Daniela Burnes Vargas
A Saccadic Adaptation task that can be done at home.
Diffuse Optics Team
Ziping Liu, Hunsuk Stefan Ha, Shenglin Liu
A system to apply diffuse optical imaging to monitor fracture healing in the foot.
Polymer Surface Modification to Augment VITROS® MicroWell Technology
Geoffrey Rouin, Jingyi Fan, Alessandro Del Priore
Polymer to enhance capture molecule binding on MicroWell surface for increased assay.
The Listen'Ears
Arushi Jain, Salah Mahmoudi, Jacques Kouevi, Jeremy Deniega Using modern technology to analyze brain-ear interfaces to help you listen to what really matters. 
TouchStream Seizure Detection
Icxel Valeriano, Hetince Zhao, Michiko Feehan, Jingxia He
The design of an algorithm capable of detecting seizure onset, duration, and severity.
IV Easy
Julia Herman, Hyun Woo Kim, Hong Chen
To assist nurses and reduce human errors by hospital bedsides related to IV tube connections.
Early Mobility for Kids
Joseph Cappotelli, Daniel Myers, Hyun (Jennifer) Choi, Devon Foggio
The creation of an early mobility system for children with developmental disabilities. 
Dia-Beat-It
Sue Zhang, Matt Boulanger, Jack Hayden, Fredella Lee
A point of care screening device for type 2 diabetes.
TB Skin Deep
Anli Lin, Tianyu Wu, Raymond Chin, Alexander Strand
Developing an improved method of diagnosing TB using PPD
Center for Medical Technology & Innovation (graduate students)
Aortic Wall Exposure
Students: Connor McBride, Emily Newman, Josh Schum-Houck
Clinicians: Dr. Spencer Rosero, Dr. Peter Knight, Dr. Bryan Barrus
Our device will be used during minimally invasive aortic valve replacement surgeries to aid in the exposure of the aortic valve tissue area and allows for easier implantation of the replacement valve. This improvement will make performing minimally invasive surgeries more accessible to surgeons.
Quick and Repeatable Ultrasound Imaging during CPR
Students: Vladimir Tokarchuk, Eric Ravinal
Clinicians: Dr. Lu, Dr. Miglani, Dr. O’Connor, Dr. Rosero
A way to reduce the time needed to find the right ultrasound image in cardiac arrest patients, in order to minimize the time that the patient’s brain is not receiving oxygenated blood.

Dural Safe Bone Removal
Students: Amanda Smith, Evan Sosnow, Rebecca Amorese
Clinicians: Dr. Addisu Mesfin, Mr. Robert Molinari, Dr. Paul Rubery
A way to enable the surgeon to use both hands on the Kerrison Rongeur while simultaneously cutting, removing and collecting targeted bone segment during lumbar decompressions in order for the surgeon to safely and effectively carry out the procedure.
CompreSure’s Compressive Intramedullary Rod (CIMR) System
Students: Meghann Meyer, Gregory Dadourian, Alyssa Lopez
Clinicians: Dr. Gorczyca, Dr. Dave Ciufo
A new implant that allows for minimally invasive fracture fixation and compression of breaks located in the humerus. Our novel technology utilizes controlled compression of the fracture site to promote faster and stronger bone healing, which leads to improved patient recovery.

( back to top)
Class of 2017
2017 BME Photo Gallery on FacebookSeniors
ASAP: Automated Sigma Analysis Platform
Our team has been working with Baxter to improve optical and software techniques to quantify flow rate of their Sigma Spectrum drug infusion pump. Current methods for flow rate calibration of hospital infusion pumps are subjective and prone to errors such as evaporation. Developing an accurate and thorough calibration set-up can be tedious, costly, and space-inefficient. We have developed a novel, inexpensive calibration device to validate infusion pump flow rate intended for use in research and development, and quality assurance of Baxter’s pumps.
Team members: Morgan McDonald, Winslow Powers, Claire Kaiser, Ge Song
Supervisor: Richard Waugh, PhD, Biomedical Engineering, UR
Customer: Baxter International, supervised by Matt Bivans
Cable Medical ECG Cable Adapter
In a hospital environment, time is a commodity. Currently, hospital workflow is impeded by clinicians’ need to change ECG systems as a patient moves through the hospital throughout their stay. We aim to modify Curbell Medical's existing ECG cable system in order to limit disruptions to clinical workflow and minimize the hospital’s waste caused by discarding incompatible lead sets. The solution consists of a permanently attached, optimized cable-adapter module which enables smooth navigation through hospital-identified critical pathways.
Team members: Connor O'Brien, Raiem Smith, Madison Schumacher, Vladimir Tokarchuk
Supervisor: Regine Choe, PhD, Biomedical Engineering, UR
Customer: Mike Regan and Don Gibson, Curbell Medical
Sepsis Detectis Team

Our team is working to combat the drastic hospital mortality rates of sepsis by developing a faster detection technology. We aim to implement hyperspectral imaging as a non-invasive diagnostic tool for use within an intensive care unit. Instead of conducting cell cultures and blood tests, which are both invasive and time consuming, the goal of this device is to help detect and quantify the presence sepsis in minutes.
Team members: Kathleen Larson, Dylan Latham, Justin Schumacher, Brittany Schutrum, Joshua Schum
Supervisor: Dr. Catherine Kuo
Customer: W. Spencer Klubbens
CTEV Brace Team

Our team has been tasked with creating a better brace to treat CTEV (clubfoot), a congenital deformity where a child is born with their feet turned inward and upward. The current method, the Ponseti Brace, is a boots and bar system with many drawbacks. Aside from restricting movement, it’s uncomfortable and difficult for parents to use. As a team we have created a barless alternative brace that is lighter and more comfortable, while also tracking patient compliance. We hope that our brace can be used to improve the lives of children with CTEV and their parents everywhere.
Team members: Genevieve Caldwell, Ka-Kyung Kim, Matt Stein, Mingyang Mao
Supervisor: Catherine Kuo, PhD, Biomedical Engineering, UR
Customer: Dr. Kuo, Department of Biomedical Engineering, UR and Dr. O'Malley, Department of Orthopedics, UR
Diabetes in Micronesia
Micronesia is a region in the Western Pacific made up of island nations, including the Republic of the Marshall Islands and Federated States of Micronesia. Approximately one-third of individuals in these countries have type 2 diabetes. Our team has developed a tablet-integrated toolkit that facilitates the collection and analysis of biometric data for local community health workers. We consider unique social circumstances in the region to guide community health workers in creating effective individual health plans for their patients
Team members: Tristan Ford, Raaga Kanakam, Omar Soufan, Tyler Vasquez-Dorn
Supervisor: Edmund Lalor, PhD, Biomedical Engineering, UR & Trinity
Customer: Timothy Dye, PhD, CTSI; Ivelisse Rivera, MD, CTSI; Jose Perez-Ramos, MPH, CTSI
Dialysis Patient Simulator Team

Fresenius Medical Care is a leading provider of hemodialysis products and services, treating more than 300,000 patients worldwide. Currently, there is no product that can perform patient simulations for new dialysis machine prototypes. Our device interfaces with a hemodialysis machine just as a patient would in order to simulate changes in fistula blood pressures, hematocrit, and oxygen saturation. It also monitors these pressures, bloodline flow rate, and dialysate temperature to ensure that the sensors and responses within the prototype are correct.
Team members: Runxuan (Sophia) Zhao, Rebecca Lewis, Marina May, Fengyi (Arthur) Jiang
Supervisor: Dean Johnson, PhD, Biomedical Engineering, UR
Customer: Mike Owen, Fresenius Medical Care
Dynamic Wheelchair
In order to help patients with spinal cord injury avoid pressure sores, we have endeavored to revolutionize wheelchair seating. By sensing and recording a user’s current position and pressure distribution our device will assess and adjust the pressure in a seat to prevent the high pressure regions that cause pressure sores. As a mechanically operated adjunct to the ROHO cushion, this customizable sleeve will fit neatly over a variety of ROHO cushion sizes and types.
Team members: Albert Chen, Maddy Cappelloni, Greg Dadourian, Shannon Fitch
Supervisor: Hani Awad, PhD
Customer: Dave Whalen
Glucometry for the Visually Impaired Team
Currently, 28.5% of Americans over the age of forty have some degree of visual impairment due to diabetes. The Glucometry for Visual Impairment team hopes to create a more effective way for patients with diabetes and visual impairment to get a blood sugar reading. In collaboration with Joel Benzel of Touchstream Solutions, we have created a plastic ring with guides for lancets and glucose meter test strips to simplify the process of checking blood sugar for patients with visual impairment.
Team members: David Tannenbaum, James Melton, Brenna Schnell, Janice Youwen Xia
Supervisor: Anne Luebke, PhD, Biomedical Engineering, UR
Customer: Joel Benzel, CEO & Founder, Touchstream Solutions
ICU Ambulation Team
Ambulating with patients recovering in the intensive care unit is perceived as a difficult task with all the medical devices necessary to monitor vital signs. Our goal is to deliver a physical therapy aid for patient ambulation in the intensive care unit at URMC. The physical therapy aid will focus on providing the patient with lateral support and stability while also carrying the medical devices necessary to monitor the patient vital signs during ambulation. The design of the physical therapy aid will ensure that patients can safely walk with a normal stride length
Team members: Katherine Konopka, Jeffrey Greblick, Tyler Cavanaugh, Minsoo Kim Katherine Konopka, Jeffrey Greblick, Tyler Cavanaugh, Minsoo Kim
Supervisor: Jim Mc Grath, PhD, Biomedical Engineering, UR
Customer: Kathy Owens, Department of Physical Therapy, URMC
OPTI (Optimal Photoacoustic Transmission Imaging) Phantom Team
Photoacoustic Imaging (PAI) is an imaging modality that combines both optical near-infrared and ultrasonic imaging. For PAI to be implemented in the clinical environment, there must be a reproducible method for calibrating and verifying the imaging system parameters. Our team is developing a phantom that will model the imaging of blood vessels in human tissues. These phantoms will be used to determine the spatial resolution of Dr. Navalgund Rao’s PAI system for imaging vessels of varying depths and diameters
Team members: Zachary Sia, Nick Vohra, Amanda Smith, Vincent Ching-Roa
Supervisor: Steve McAleavey, PhD, Biomedical Engineering, UR
Customer: Dr. Navalgund Rao, Research Professor, Chester F. Carlson Institute for Visual Science; RIT and URMC
Pediatric Assisted Locomotion System (PALS)

We are working with local pediatric physical therapists Kelly Gilroy and Leah Talbot to design a PT system to teach children with motor delays resulting from Down syndrome and cerebral palsy to walk. Children with motor delays learn to walk a year late on average, and because of this, tend not to hit developmental milestones on time. Our treadmill-based supportive gait trainer aims to teach these children to walk earlier, giving them more independence and the capability to explore and learn about their surroundings.
Team members: Alex Kazmierczak, Courtney Semkewyc, Jolan Burger, and Nitish Sardana
Supervisor: Mark Buckley, PhD, Biomedical Engineering, UR
Customer: Leah Talbot, MSPT, Roosevelt Childrens Center and Kelly Gilroy, PT, DPT
Pediclear
During spinal fusion procedures, surgeons need a better way to detect defects in the pedicle tract in order to determine whether it is safe to implant pedicle screws. We designed a surgical probe, Pediclear, that senses changes in vibration pattern as it moves against the walls of the pedicle tract and alerts the surgeon to the presence of a breach. The solution adds certainty to breach detection, reduces false positive rates, and aids in resident training without adding extra time, equipment, and cost to the procedure.
Team members: Spencer DeCinque, Kerry Donnelly, Saadedine El-Homsi, and Brittany Garrison
Supervisors: Amy Lerner, Ph.D, Greg Gdowski, Ph.D, Martin Gira, M.S., Biomedical Engineering UR
Customers: Addisu Mesfin, Orthopaedic Surgery, Paul Rubery, Chair of Department of Orthopaedics and Rehabilitation, James Sanders, Chief of Pediatric Orthopaedics, and Kenneth Foxx, Spine Fellow, UR Medicine
Proteus Medical

Canines are the most common offenders of consuming foreign bodies, requiring a veterinary visit to remove the object to prevent further harm. Endoscopic retrieval is the preferred method of extracting these foreign bodies. However, endoscopic retrieval devices on the market today are neither robust nor reusable, often deforming after single use. At Proteus Medical, our team has developed a unique design that will reduce both the retrieval time and yearly expenditures. Together, we aim to revolutionize the endoscopic retrieval field through our novel device.
Team members: Edward Ruppel III, Chandler Woo, Connor McBride
Supervisor: Diane Dalecki, PhD and Department Chair, Biomedical Engineering, UR
Customer: Erika de Papp, DVM, DACVIM, MSPCA-Angell, Boston, Massachusetts
Sample Illumination Team
Ortho Clinical Diagnostics currently produces a line of immunodiagnostic systems to analyze the chemistry of patient's blood samples using reflectometry. In order to provide a more confident analysis of these samples, our team is developing an illumination system that delivers a more uniform plane of light to the blood sample while also being more robust, reliable, and less expensive.
Team members: Hamilton White, Joseph Malone, Kasey Kwong, Danny Capucilli
Supervisor: Ed Brown, PhD, Biomedical Engineering, UR
Customer: Bob Jones, Ortho Clinical Diagnostics
Sensor Skin for Robotics
The Sensor Skin for Robotics team aims to design a sensory system for a robotic hand to assist the robot in making successful attempts when grasping objects. The system must be capable of detecting contact forces upon a grasping attempt, determine the success of the attempt, and be capable of relaying this information to the robot’s operating system. Thus we intend to design a sensor-skin system with secondary signal processing to meet these criteria.
Team members: Kushael Chakravorty, Ben Abbatematteo, Peter Burlingame, Hyeon Woo Lee, Yesubet Dereje
Supervisor: Ross Maddox, PhD
Customer: Thomas Howard, PhD
Staple Removal Team
Our project aims to redesign the standard staple removal process. Employees at Lifetime Assistance Inc. are required to remove staples from documents for up to six hours a day as part of a larger scanning, archiving and shredding operation. Through the redesign of a staple remover and adding a staple collection and staple detection system, we hope to make this process easier and faster
Team members: Rahul Upadhya, Mara Lanis, Kevin LeBlanc
Supervisor: Scott Seiman, PhD, Biomedical Engineering, UR
Customer: Martin Reeners, Lifetime Assistance Inc.
S.T.A.R.S: Scoliosis Phantom

Adolescent idiopathic scoliosis is defined as a lateral deviation of the spine which is also commonly associated with rotation of the vertebrae. The Scoliosis Phantom is a realistic model of the lumbar region of a scoliotic spine for an adolescent female patient suffering from idiopathic scoliosis. Our phantom will serve as a research tool to increase the repeatability and reliability of the brace-making process by reducing the number of brace fittings and X-Ray scans a patient will have to undergo.
Team members: Andrew Arjana, Rebecca Amorese, Shamroz Farooq, Stephanie Kamau, Tongxi Zhuang
Supervisor: Amy Lerner, PhD, Biomedical Engineering, UR
Customer: James Sanders, M.D. Chief of Pediatric Orthopaedic Surgery, URMC, Sean Zeller, MBA, MSPO, CPO Chief, Orthotics and Prosthetics Program, URMC
Ther DermWell System Team
Transdermal Drug Delivery (TDD) provides a valuable alternative to traditional drug delivery methods, due to its potential to decrease biohazardous waste production and improve overall accessibility. In collaboration with the URMC dermatology department, we have developed a novel system for testing a novel TDD method which involves a reagent that temporarily increases the permeability of the skin, allowing for large molecule drug delivery such as a vaccine.Our device is a low cost, user friendly R&D tool for testing on human skin biopsies
Team members: Breanna O'Reilly, Samantha McGoldrick, Chris Cook, Comfort Adeyemi, Arun Nambiar
Supervisor: Danielle Benoit, PhD, Biomedical Engineering, UR
Customer: Ben Howard, PhD, Department of Dermatology, URMC
Tympanic Membrane Visualization
Due to the prevalence of ear infections - especially in young children - and the potential risks of misdiagnosis, we are developing a device with our customer, URMC Otalaryngologist Dr. John Faria, to allow clinicians to more effectively diagnose this condition through better visualization of the tympanic membrane and the ability to acquire images through a computer interface
Team members: Janet Sorrells, Nathaniel Barber, Kathryn Maisch, Tina (Haitong) Wang
Supervisor: Anne Luebke, PhD, Associate Professor of Biomedical Engineering and Neuroscience, UR
Customer: John Faria, M.D. Department of Otolaryngology, URMC
Center for Medical Technology & Innovation
CMTI Orthopaedics Team
During spinal fusion procedures, surgeons need a better way to detect defects in the pedicle tract in order to determine whether it is safe to implant pedicle screws. We designed a surgical probe that senses changes in vibration pattern as it moves against the walls of the pedicle tract and alerts the surgeon to the presence of a breach. The solution adds certainty to breach detection, reduces false positive rates, and aids in resident training without adding extra time, equipment, and cost to the procedure,
Team members: Spencer DeCinque, Brittany Garrison, Saadedine El-Homsi, Kerry Donnelly
Supervisor: Greg Gdowski, PhD, Center for Medical Technology & Innovation and Amy Lerner, PhD, Center for Medical Technology & Innovation
Customer: Spinal Surgeons
EyePidural: An Optical & Pressure Feedback Device to Improve Epidural Procedures
Epidural procedures, a method of pain alleviation, involve blindly placing a needle through a patient's back into a small, thin epidural space above the spinal cord. Our device, the EyePidural, is a hybrid optical and pressure feedback system that relies on color variations and pressure differences from the spinal tissue layers. These differences will help guide the needle to the epidural space safely and accurately without causing undue injury, reducing procedural complications and increasing patient and physician peace of mind.
Team members: Bethany Lennox, Caeli Quiter, and Courage Tsiagbe
Supervisor: Greg Gdowski, PhD, Biomedical Engineering, UR; Amy Lerner, PhD, Biomedical Engineering, UR; Martin Gira, Biomedical Engineering, UR
Customer: Daryl Smith, MD, Anesthesiology and Pain Service, UR Medicine
InstaTract: Atrial Retractor for Minimally Invasive Mitral Valve Surgery
Our team is developing a novel atrial retraction device for use in minimally invasive heart valve surgery. Current atrial retractors have a significant learning curve and either create an extra incision through the chest wall and risk bleeding, or take up valuable space in the surgeon’s field of view. The InstaTract is an intuitive and quickly deployable device that provides retraction of varying size atria, exposing the valve being repaired or replaced.
Team members: Ian Baranowski, Margaret Ferrari, Kyle Meyers, Lauren Seitz
Supervisor: Greg Gdowski, PhD, Biomedical Engineering, UR; Martin Gira, Biomedical Engineering, UR; Amy Lerner, PhD, Biomedical Engineering, UR
Customer: Fabio Sagebin, MD, Cardiothoracic Surgery, UR
( back to top)
Class of 2016
Seniors
Ultranomics
Greg Palis, Megan Routzong, Yanwen Zhai, Mary Bucklin
The vast majority of ultrasound sonographers require treatment for Musculoskeletal disorders caused by repetitive, improper ergonomics while at work. We aim to monitor and log the kinetics, kinematics, and position of sonographers’ upper extremities continuously throughout all procedures they conduct and provide this information to employers. The data collected must elucidate the source of injury and eventually assist with guiding preventative measures.
TouchStream Solutions Medication Management
Jacob Parisi, a senior in Biomedical Engineering, works on his team's senior design project, to create a medication dispenser integrated with the current TouchStream scheduling system. Photo by J. Adam Fenster/University of Rochester.
Hayley Forrest, Brittany Garrison, Bethany Lennox, Rachel Melnyk, Jacob Parisi
Our project addresses the problems identified by TouchStream Solutions with the current pillbox for use with their medication scheduling system. We created a medication dispenser integrated with the current scheduling system that can be customized for various medications and customer needs for patients including individuals with mental disabilities and those above age 65. This medication dispenser will help improve customer interaction with the TouchStream system, assist customers with the management of daily medications and reduce instances of incorrect medication doses.
Customer: Joel Benzel, TouchStream Solutions
Supervisor: Rick Waugh, Ph.D., Biomedical Engineering, University of Rochester
Team BAXTER
Saadedine El-Homsi, Bennett Nidenberg, Yuxin Teng, Dylan Hoffman
The height of an intravenous bag in relation to the attached infusion pump is capable of impacting the amount of medicine the system delivers. If the height difference is inappropriate, the scenario has potential to lead to lower success rates for treatments and further complications. By developing a mechanism to ensure that the height is consistently within a tolerable range of the ideal value, we aim to increase accuracy of infusions and reduce the risk to patients from incorrect dosages.
Customer: Matt Bivens, Baxter Healthcare
Supervisor: Danielle Benoit, Ph.D., Biomedical Engineering, University of Rochester
ECG LeadURs
Taryn Amatruda, Jack Venuti, Jonathan Boualavong, Kyle Meyers
We aim to design an ECG lead wire that is capable of providing reliable ECG signals by connecting to tab and stud electrodes securely. The lead wire connection must be inexpensive to manufacture, efficient to sanitize, and comparable to market alternatives in ease of use and patient comfort. Most importantly, the ECG lead must increase electrode retention in an effort to minimize the alarm fatigue and inefficient ECG monitoring occurring in clinical settings worldwide.
Customer: Theresa Hart, Curbell Medical Products, Inc.
Supervisor: Scott Seidman, Ph.D., Biomedical Engineering, University of Rochester
Fetal Cardiac MRI
Alex Choy, Andrew Graveley, Kevin Jin, Tae Jun Yoon
MRI is the best option for diagnosing potential issues in fetal hearts, as the technology provides high resolution and lacks harmful ionizing radiation. However, MRI is limited due to the inability to measure the fetal heartbeat for selectively timing the image acquisition. By designing a device that can safely obtain an accurate fetal heart rate and communicate this information to the MRI machine without interfering with the imaging process, we aim to improve diagnosis of congenital heart defects before birth.
Customer: Mitchell Chess, M.D., Associate Professor, Diagnostic Imaging, UR Medicine
Supervisor: Stephen McAleavey, Ph.D., Biomedical Engineering, University of Rochester
Dialysim
Alycia Abbot, Zachary Jenkins, Ryan Spooner, Justin Delafontaine
Our product will act as a verification and validation device in a laboratory testing environment for Fresenius’s Dialysis Equipment. It will interface with the hemodialysis system and have the ability to simulate changes in blood pressure, blood temperature, and oxygen saturation and hematocrit. This will allow Fresenius to examine their equipment’s response to changes in the state of our model.
Customer: Dirk Stevens, Fresenius Medical Care
Supervisor: James McGrath, Ph.D., Biomedical Engineering, University of Rochester
Braille Reader Team

Matthew Mender and Emily Kwan work on the Braille Reader they developed with fellow team members Christina Amaral, Emma Gira and Kevin McAlpine. (Photo by J. Adam Fenster/University of Rochester)
Christina Amaral, Emma Gira, Emily Kwan, Kevin McAlpine, Matthew Mender
Seventy two percent of people with diabetes will develop diabetic neuropathy by their mid-fifties. For individuals who are visually impaired, the onset of severe diabetic neuropathy means they can read neither visually nor tactilely, through the use of braille. Our mission is to develop a device that will translate the braille documents of a person with diabetic neuropathy into an accessible output. Additionally, we envision this device as an aid to non-Braille readers in inclusive educational and workplace environments.
Customer: Joseph Kells, ABVI -Goodwill
Supervisor: Laurel Carney, Ph.D., Biomedical Engineering, University of Rochester
TripP: Primate Positioning People
Caeli Quiter, Zhou Xu, Thomas Varner, Erik Page
We aim to design and fabricate a new head positioning apparatus to be used for retinal imaging in primates for the Advanced Retinal Imaging Alliance (ARIA). The apparatus must include precise pitch and azimuth rotation about the pupil, a safe way to position the primate, improved stability, and the ability to interface with ARIA’s imaging systems.
Customer: Jennifer Hunter, Ph.D., Advanced Retinal Imaging Alliance
Supervisor: Mark Buckley, Ph.D., Biomedical Engineering, University of Rochester
D.A.N.I. (Dynamic Anthropomorphic Innovation) Phantoms
Sandra Oluoch, Chris Plunkett, Jenny Quintero, Susan Butler
Carestream Health, a provider of radiography equipment, has expressed difficulty assessing the performance of its imaging equipment using conventional radiographic phantoms. As such, this project was established to perform modifications to an existing phantom to measure dynamic latency, simulate flow and show sufficient contrast between flowing substances & surroundings.
Customer: Sam Richard, Ph.D, Senior Research Scientist, Carestream Health
Supervisor: Regine Choe, Ph.D., Biomedical Engineering, University of Rochester
Pot Skirt Team

The Pot Skirt team tests their prototype. From left, YeJin Jeong, Nikki Sroka, Jessica He, and Adam Langenbucher. Photo by J. Adam Fenster/University of Rochester.
Jessica He, Adam Langenbucher, Nikki Sroka, YeJin Jeong
Due to dangers in deforestation, toxic byproduct emission, and financial strains for families in Kenya, there is a strong demand for pot skirts that can increase fuel efficiency by improving convective heat transfer in cookstoves. Consumers have also requested that the pot skirt be adjustable to several pot sizes. In correspondence to these customer needs, we have created a pot skirt design that is safe, cost effective, fuel-efficient, adjustable and is compatible with the upcoming line of wood-burning BURN cookstoves.
Customer: Paul Means, Research and Testing Manager at BURN Stoves
Supervisor: Amy Lerner, Ph.D., Biomedical Engineering, University of Rochester
Vestibular Vibes
Yuqi Wu, Luke Daily, Ian Baranowski, Allison Stiller, Tristan DeAlwis
Benign Paroxysmal Positional Vertigo, BPPV, is a condition caused by detachment of otoconia (calcium carbonate crystals) from the otolith organs and subsequent migration of otoconia into the semicircular canals. Presence of these otoconia creates a false sense of acceleration in the patient by stimulating the vestibular hair cells, thus causing nausea and vertigo. Therefore, we intend to design a vibrational device that can be applied to the mastoid of the patient in order to deliver oscillations capable of breaking apart the clumped otoconia.
Customer: Benjamin Crane, M.D., Department of Otolaryngology, UR Medicine
Supervisor: Anne Luebke, Ph.D., Biomedical Engineering, University of Rochester
Wrist Support Team
Aaron Ketting-Olivier, Tianyi Lu, Erica Hange, Marshal Davidson, Christian Freitas
Individuals with wrist paralysis struggle with daily tasks that involve the manipulation of their environment and subsequently rely heavily on others for help. We have created a line actuated wrist brace that allows the user to perform a lateral pinch.
Customer: David Whalen, JD
Supervisor: Jong-Hoon Nam, Ph.D., Mechanical Engineering & Biomedical Engineering, University of Rochester
Scoliosis Brace Compliance
Marlen Mahendraratnam, Evan Sosnow, Samuel Perakis, Amanda Tian, Nathan Sowards
For adolescent Idiopathic Scoliosis children between the ages of 10 and 15 years old, bracing has been shown to be effective at stopping curve progression and preventing unnecessary surgery. Due to low compliance, only a fraction of children get the full benefit of bracing. Our group seeks to increase patient compliance & thereby bracing efficacy by addressing patient concerns with current braces & bracing techniques.
Customer: James Sanders, M.D., Pediatric Orthopaedics, UR Medicine
Supervisor: Hani Awad, Ph.D., Biomedical Engineering, University of Rochester
Endosign
Natalie Tjota, Gina DeMeo, Matt Todd, Sydney White
Gastrointestinal endoscopies are the most frequently performed outpatient procedure in the United States, and the country’s aging population calls for a more efficient procedure. The procedure requires a gastroenterologist to feed biopsy forceps through the endoscope channel and back repeatedly, which is unnecessarily time consuming. The goal of our project is to reduce the passing time of the forceps through the instrument channel of the endoscope.
Customer: Truptesh Kothari, M.D., M.S., Gastroenterology/Interventional Endoscopy, UR Medicine
Supervisor: Ed Brown, Ph.D., Biomedical Engineering, University of Rochester
AnesthEZ Nerve Block Improvementa
Jake Gusman, Syed “Reefat” Aziz, Estefania Garza, Rose Mbaye
Currently nerve block procedures require the presence of two anesthesiologists; the first being in charge of holding the ultrasound probe and guiding the needle, the second pressing on the syringe plunger to either dispense or aspirate anesthetics. The objective of our project is to improve the efficiency of the nerve block procedure by replacing the second anesthesiologist with a footcontrolled syringe pump and thus reducing the procedure to a one-person job.
Customer: Daryl Smith, MD, UR Medicine
Supervisor: Catherine Kuo, Ph.D., Biomedical Engineering, University of Rochester
Center for Medical Technology & Innovation
ScolioFit
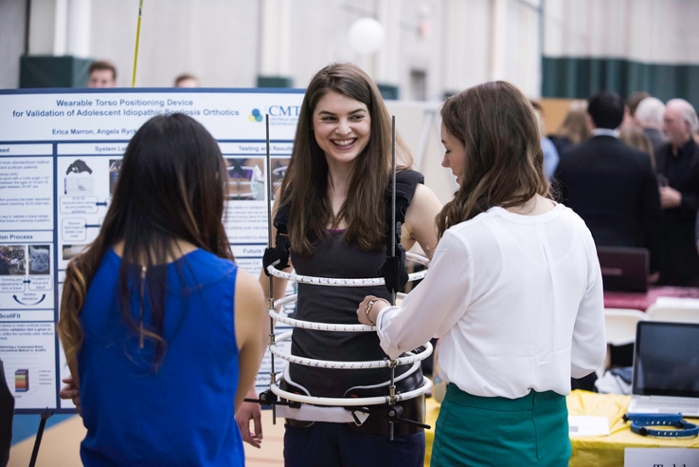
Angela Ryck demonstrates "Scoliofit"
Erica Marron, Angela Ryck, Danielle Wilson
Our mission is to help orthotists create the optimal brace for each patient’s unique spinal curvature. ScoliFit is a wearable torso-positioning device designed for use on adolescent idiopathic scoliosis patients. This device can determine the torso position that immediately reduces a given patient’s spinal curvature and enables orthotists to incorporate that position into the profile of the patient’s final brace. Since the current method of making braces is subjective and has no such capacity for validation, ScoliFit is unique in its ability to establish the optimal brace design before the brace is made.
Customers: Dr. James Sanders, MD, Orthopaedics M&D, UR Medicine and Sean Zeller, Chief Orthotics, Orthotics and Prosthetics, UR Medicine
Supervisors: Dr. Greg Gdowski, Ph.D, Executive Director, Center for Medical Technology and Innovation (CMTI) , Dr. Amy Lerner, Ph.D., Academic Director, CMTI, Martin Gira, Senior Research Engineer, CMTI
Advanced Medical Draining Technologies
Tristan Richardson, Kayleigh Miller
We are developing a product to be used in conjunction with surgical drains in order to improve fluid removal from post-surgical cavities after invasive procedures, which will reduce the incidence of costly surgical site infections. The device consists of a porous, bio-absorbable mesh, allowing for tissue ingrowth, with a drain pattern throughout. It is placed during patient closure, functions while the drain is in place and then degrades over time. Novel 3D printing technology will be utilized.
Team Members: Tristan Richardson, Kayleigh Miller
Customers: Dr. Howard Langstein and Dr. Peter Koltz, UR Medicine
Supervisors: Dr. Greg Gdowski, Ph.D, Executive Director, Center for Medical Technology and Innovation (CMTI) , Dr. Amy Lerner, Ph.D., Academic Director, CMTI, Martin Gira, Senior Research Engineer, CMTI
StimSense
Martin Gitomer, Shwe Pyie
Our device aims to quantitatively monitor levels of neuromuscular blockade in patients undergoing surgery. Neuromuscular blocking drugs are used as muscle paralytics to prevent patients from reacting to surgical stimuli. Currently, anesthesiologists subjectively monitor dosing of neuromuscular blockade. Our device objectively monitors neuromuscular blockade throughout surgery to guide proper dosing, reduce post-op complications and achieve better recovery.
Customers: Dr. Michal Eaton, Dr. Raymond Zollo, Dr. Daryl Smith, UR Medicine and George Anstadt
Supervisors: Dr. Greg Gdowski, Ph.D, Executive Director, Center for Medical Technology and Innovation (CMTI) , Dr. Amy Lerner, Ph.D., Academic Director, CMTI, Martin Gira, Senior Research Engineer, CMTI
Intelligent Cooler Enterprise (ICE): Our mission is to create a more robust device for blood transportation within hospitals while decreasing the workload of employees. Our insulating device can measure the temperature of its contents and keep blood within the regulated temperature range significantly longer then the current system. Our product can also connect to a network so that we can notify personnel of unexpected temperature events, and in turn create a safer, more efficient hospital for patients that may be at risk for transfusions.
Team Members: Scott Harrienger, Andrew Zeccola
Customers: Diane Bullock Medical Technical Specialist, BloodBank-Clinical Labs, UR Medicine and Deborah Masel, Blood Bank-Clinical Labs Chief Supervisor.
Supervisors: Dr. Greg Gdowski, Ph.D, Executive Director, Center for Medical Technology and Innovation (CMTI) , Dr. Amy Lerner, Ph.D., Academic Director, CMTI, Martin Gira, Senior Research Engineer, CMTI
( back to top)
Class of 2015
Seniors
D.O.M.E. (Dome Osteotomy Medical Equipment)
Project Description: The development of surgical instruments to improve fixation in the dome high tibial osteotomy, a procedure to relieve pressure in the knee joint caused by knee osteoarthritis
Team: Meghan Kazanski, Alexander Lambropoulos, Reuben Morrison, Stacie Zwolski
Customer: Martin Korn, MD, FACS, FAAOS
Supervisor: Amy Lerner, PhD, Biomedical Engineering/CMTI, University of Rochester
SimuClage
Project Description: A simulator for OB/GYN residents at UR Medicine to practice the cervical cerclage procedure that consists of placing stitches around incompetent cervixes to prevent preterm births
Team: Maria Cazacu, Brittanie Kilchoer, Jennifer Park, Melinda Vander Horst
Customer: Christine Arnold, R.N.C., M.S., Center for Obstetrics & Gynecology, Simulation, UR Medicine
Supervisor: Anne Luebke, PhD, Biomedical Engineering, University of Rochester
AdaptaBOWL Ramp
Project Description: The AdaptaBOWL team is developing an adaptive ramp to improve the independence of recreational bowling for people with physical and mental disabilities
Team: Carrie DeMoulin, Juliana Orlov, Stephanie Rigot, Jonathan Yang
Customer: Michael Tuller CAPE, Adapted Recreation Services, Rochester NY
Supervisor: Anne Luebke, PhD, Biomedical Engineering, University of Rochester
Neonatal PICC Line Introducer
Project Description: A comprehensive and effective PICC line introducer for delivering nutrients and life-sustaining medications to neonates
Team: Jessica Chen, Hiroshi Inuzuka, Michael Silverstein, Ling Yang
Customer: Kristin Scheible, MD, Department of Pediatrics, Neonatology, UR Medicine
Supervisor: Rick Waugh, PhD, Biomedical Engineering, University of Rochester
Bladder Cancer Surgery Simulator
Project Description: A training aid for urologists performing bladder cancer surgery
Team: Kevin Fogarty, Marlin Myers, Nuley Seo
Customer: Chuck Welliver MD, Albany Medical Center, Albany, NY
Supervisor: James McGrath, PhD, Biomedical Engineering, University of Rochester
Intervertebral Endplate Preparation Device for Spinal Fusion Surgery
Project Description: To improve spinal fusion surgery through a reproducible endplate preparation
TEAM: Jarvis D’Souza, Keith Grafmeyer, Samuel Kwak, Stephen Sloan
Customer: Jeremy Malik, NuVasive, Inc., San Diego, California
Supervisor: Hani Awad, PhD, Biomedical Engineering, University of Rochester
Sonodontist
Project Description: An Ultrasonic Tooth Crack Detector
Team: Tek Gautam, Jacob Hyatt, Alexa Kuenstler, Jonathan Macoskey, Jungeun (Jenny) Won
Customer: Robert Lerner, MD, PhD, FACR, Rochester Regional Health System
Supervisor: Diane Dalecki, PhD, Biomedical Engineering, University of Rochester
Photoacoustic Imaging
Project Description: The development of an appropriate mechanical mechanism in a photoacoustic imaging device to be able to scan multiple object planes without any reduction in image quality
Team: Carlos Benitez, Rafique Khan, Emmanuel Mannoh, Benjamin Yue
Customer: Navalgund Rao, PhD and Vikram Dogra MD., Dept of Imaging Sciences, UR Medicine
Supervisor: Edward Brown, PhD, Biomedical Engineering, University of Rochester
GoVertigo
Project Description: Device to perform canalithic repositioning maneuver treatment for Benign Paroxysmal Positional Vertigo
Team: Yaron Adar, An An, Anna Gaines, Hanyang Liu
Customer: Benjamin Crane, MD, PhD, Department of Otolaryngology, UR Medicine
Supervisor: Jong-Hoon Nam, Mechanical Engineering & Biomedical Engineering, University of Rochester
RADD (Rapid Autonomic Dysreflexia Detection)
Project Description: Autonomic dysreflexia is a potentially lethal condition that occurs in people with spinal cord injuries. RADD detects dysreflexia events before they can cause any permanent damage
TEAM: Vasanthi Balaji, Harrison Clarke, Benjamin Dengler, Joseph Wagner
Customer: David Whalen, JD
Supervisor: Laurel Carney, PhD, Biomedical Engineering, University of Rochester
ChronoMed
Project Description: A portable pill dispenser attachment for PharmaAdva’s automatic medication dispenser
Team: Adam Hartman, Hang Li, Michael Mayor, Andrew Zeccola
Customer: Michel Berg, MD, Department of Neurology, UR Medicine
Supervisor: Scott Seidman, PhD, Biomedical Engineering, University of Rochester
MTDesign
Project Description: A device intended to elucidate the correlation between muscle tension dysphonia and the pressure associated with the closing of the soft palate against the posterior pharyngeal wall
TEAM: Wing Han Wilkins Cheng, Kevin Colman, Francis Cunningham, Kathryn Luly
Customer: John Ingle, MD, Department of Otolaryngology, UR Medicine
Supervisor: Regine Choe, PhD, Biomedical Engineering, University of Rochester
BPR: Breast Pump Redesign
Project Description: Modernize current breast pumps on the market
Team: Tucker Burgin, Maura O’Conor, Sameer Shamsie, Sarah Wayson
Customer: Charles Phelps, PhD, Provost Emeritus and Grandfather, Pat Shores, MBA, Entrepreneur and Mother
Supervisor: Danielle Benoit, PhD, Biomedical Engineering, University of Rochester
UR Infection Corrections
Project Description: High throughput in vitro method to quantify antibacterial properties of coatings on catheters
Team: Samuel Gullotti, Zachary Mietus, Samuel Rubin, Namita Sarraf
Customer: Keith Savino, PhD, James Bonafini Consultants, Rochester NY
Supervisor: Dean Johnson, PhD, Biomedical Engineering, University of Rochester
HYDROLIFE: Hydration Monitor
Project Description: Precisely measure changes in hydration of elderly patients to prevent the negative consequences associated with dehydration
TEAM: Matthew Baker, Jong Suk Kim, Xiaodan (Rachel) Niu, Shivaraj Shan
Customer: Joel Benzel, Founder, TouchStream Solutions, Rochester, New York
Supervisor: Mark Buckley, PhD, Biomedical Engineering, University of Rochester
M^3(Mobile Moment Monitor)
Project Description: A device to measure the knee adduction moment in a clinical environment as a measure of risk for development knee OA
Team: Christina Kim, Alexander Matthers, Xuan (Sabrina) Pan, Kylie Stengel
Customer: Amy Lerner, PhD, Biomedical Engineering/CMTI, University of Rochester
Supervisor: Stephen McAleavey, PhD, Biomedical Engineering, University of Rochester
( back to top)
Class of 2014
Biomedical engineering seniors Casey Dahlbeck, David Abplanalp, Courtney Astemborski, Chad Pickering, and Max Winkelman, the team behind Project Hemo-Box, a redesigned blood transport container for the Medical Center's blood bank.
MRPR Solutions - A MRI compatible button response box for use in fMRI research.
Team: Jesse Checkla, Daniel Grady, Deborah Cooper, Samuel Brown
ReduXX Engineering Consulting - The creation of an adaptable testing platform for Congenital Diaphragmatic Hernia patch development: By modeling the anatomy of a growing infant and surgical methods of patch implantation, the mode of patch repair failure can be determined by analyzing tension in surgical sutures over time.
Team: Jessica Yohay, Louise Bauer, Megan Stockdill, Asia Natasha Ingram
ActiviTrend - A system to record accelerometry data and a software algorithm to analyze and display intensity levels.
Team: Jonathan Cyganik, Eugene O’Hanlon, Alin Ponici, Adam Pacheck
Set-In-Bone - To find a minimally invasive surgical securement method for subcutaneous cochlear implant signal receiver/nerve stimulator.
Team: Zee Fanek, Anthony Bianchi, Christian Weber
SkinSafe Solutions - The development of a urinary catheter securement device that can adhere to the delicate skin of ICU patients without causing blisters, skin tears or infections.
Team: Russell Adams, Ripa Chowdhury, Jacqueline Gardner, Taylor Guinan, Kristen Harding
Phantomize Designs - A model eye that mimics the optical properties of the human lens and multi-layer retina for use in Adaptive Optics (AO) ophthalmic imaging at the University of Rochester Center for Visual Sciences.
Team: Gwen Musial, Taylor McKenty, Scott Levy
BetaBird Medical - A portable continuous monitoring device for the early detection of malaria and other life-threatening diseases in small children.
Team: Dena Rothman, Benjamin Vespone, Ioannis Zampetakis, Ruobing (Frank) Qian
OSFORTIS - A mechanical cutting guide for consistent femoral neck osteotomy.
Team: Breanna Padasak, Jonathan Tran, Adin Reisner, Brandyn Devanney
Hemo-Box - Blood Storage and Transportation Cooler– A device labeled specifically for patients that can effectively store, transport, and monitor the temperature of blood in an FDA regulated storage temperature range to patients in need of a blood transfusion in the hospital.
Team: David Abplanalp, Courtney Astemborski, Chad Pickering, Max Winkelman, Casey Dahlbeck
UR DermMates - Improve the functionality and ease of use of a device that assays the skin barrier integrity of exvivo epidermis samples.
Team: Amanda Chen, Kyle Fedorchak, Qihui “Fiona” Pu, Jacob VanderBurgh
PDGP Home Watch - A long-term home monitoring system comprised of a tri-axial accelerometer and software capable of detecting falls and measuring parameters associated with fall risk and medication efficacy for people with Parkinson’s disease.
Team: Tim Felong, Le Wang, Alex King and Jiashu Li
EncapsuPeel - A new laparoscopic myomectomy morcellation device design focused on reducing procedure time and risk of fibroid pieces loss in women.
Team: Ben Faiga, Tiffany Kobee, Janice Lee, Kyle Mecca, Karen Meess
Airbrasion - A prototype wound debridement system that uses air jets and antiseptic microparticles to remove debris and necrotic tissue to promote healing.
Team: Allayna DeHond, Hyun Jin Kim, Caitlin Koski, Matthew LeVasseur, Kevin Wong
Envision Engineering - The development of a portable and unobtrusive outpatient device to continuously monitor intraocular eye pressure in order to capture trends and patterns that might allow clinicians to better diagnose glaucoma.
Team: J. C . Billone, Raghashree Rajaravivarma , Nick Rohaidy, Vincent Sayseng
Sensum Medical - The centralization and specification of alarm signals on in-patient hospital floors through a system that consolidates signals from independent monitoring devices and alerts the caregiver using a non-audible signal in order to reduce the common issue of alarm fatigue.
Team: Ellen Boland, Ariana Goodman, Danielle Jaman
Sani-Drape Systems - The development of a sterile drape that will adjust to any size gantry to create a sterile environment within the CT scanner. This will provide an environment conducive for performing parts of a biopsy procedure with the patient inside the CT scanner.
Team: Noah Elkins, Joseph Tocha, Bridgetta Ryan, Nick Benedetto
MAVAC - The development of a live-feedback system that will decrease the number of screws misplaced during the spinal fusion surgery. Team: Andrea Lee, Cyrus Lambotte, Mercy Nyamewaa Asiedu, Vincent Alleluia, Alan Rosales
( back to top)
Class of 2013
2013 Video: Hajim Senior Design: Innovation Through Interdisciplinary EducationAudioMetricResearch: Startle audiometer for research of neural processes affiliated with age-induced hearing loss
Gabor Domain Optical Coherence Microscopy Skin Scanners: Refinement for dermatology applications
URine Control: A handheld urinal for female patients restricted to bed
telyCycle: A wearable device which measures physiological signals and relays them between cyclists
ViscQuik: A device to improve consistency in mixing thickened liquids to be consumed by patients with dysphagia
DyDATS System: Device to automatically track type, dosage and time of injection of IV drugs during surgery 2nd Place Forbes*
EZ-Arm: Arm support device for stroke and TBI rehabilitation to restore arm strength for daily activities
VenAer: A guidewire for the detection of air in the heart to reduce risk of life-threatening complications in surgery
Gotcha’ Back: Postural support system combining an adjustable back support with a feedback system
Adjustable Size Pigtail Catheter: An adjustable size drainage catheter to reduce clogging and need for changes
RENDEra: Micropenned RF balloon catheter for renal denervation
Fontannula: A cannula to optimize flow in the Fontan intersection and allow connection to Ventricular Assist Device
( back to top)
Class of 2012
ProBal: In-Therapy proprioception and balance training device for rehabilitation from stroke
BrIm Box: A positioning device used during intra-operative breast tissue imaging for lumpectomy procedure
SteriBot Systems: Customized sterile environment for robotic multiprobe device
FloMaR: Surgical IV fluid administration in adults: Measurement and recording without a pump 2nd Place Forbes*
H.U.A.: Computerized self-tests of Auditory Fitness for Duty screening for hearing loss in the Armed Forces
HemoGlove/HemoPad: Fecal occult blood testing unit for detecting blood in patients' stool
MONO-MANO: A one-handed cycling control device to accommodate users with only one functional arm. 1 stPlace Forbes*, continued through Innovocracy Fund as a student-run company
AMTAC: Adjustment Mechanism for the Transfer to Adaptive Cycles
pHOX: Simultaneously monitoring of esophageal pH and blood oxygen desaturation
HLHS: Pulmonary Hemodynamic Model of Hypoplastic Left Heart Syndrome
Accufeed: Sterile media transfer from IV bags in accurate, user-defined volumes for use in cell and tissue culture
RedCat: LED-based system for biliary catheter sterilization utilizing photodynamic therapy
VertiGone: Head mounted device to facilitate the remote diagnosis of Benign Paroxysmal Positional Vertigo
( back to top)
Class of 2011
2011 Video: Design Day 2011simIV: Physiological accurate, quantitative feedback for better understanding of intravenous catheter complications
UR Walking: Linear track for gait rehabilitation of scissor gait due to brain trauma
The Commode Bidet: Bidet system to facilitate independent bathroom hygiene
EyeKey: Alternatively controlled letterboard to facilitate communication for patients with locked-in syndrome
CoroFlow: Coronary artery perfusion system for excised hearts for IVUS imaging of atherosclerosis
VasoTech Systems: Physiologically accurate model of leg vasculature to evaluate clinical interventions
Electrogustometry: Portable system to evaluate taste perception through the electrical stimulation of the tongue
RoboPaedics: A novel life-sized variable size robot to model standing human sway and test a balance system
In Home DVA: System for conducting dynamic visual acuity tests for rehabilitation of vestibular hypofunction
gluComfort: A minimally invasive glucose meter evaluating SensiVida’s microneedle technology 2nd Place Forbes*
DonDoff Solutions: Safer, easier systems to don & doff back braces for post-surgical patients 2nd Place Forbes*
Cell Stretch: A two-dimensional cell-stretching device for realistic mechanical stimulation in cell-culture experiments
RespiTune: Wireless respiratory therapy device adapted from an existing digital musical instrument, the Jamboxx
( back to top)
Class of 2010
Arm EmBrace: Improved arm-brace for rehabilitation of patients with traumatic brain injury, 1st Place Forbes*
Blood Cell Bioreactor: A device producing erythrocytes through mechanical stimulation via pressure control
DiaMS: Diabetes Accessible Management System—better accessibility for patients with complications of diabetes
E.TECT E.coli Sensing System:A portable reagent-free fluorometer for detection of E.coli in aqueous environments
Fluoroprosthetic Percutaneous Intragastric balloon (FPIB):An intragastric balloon to promote weight loss
Injector Perfectors: Device to realistically model injections with collapsible veins, 3rd Place Forbes*
Limb Heater for EMG & Nerve Testing:Reusable limb temperature regulation for nerve conduction studies
Pressure Point: Localized pressure stimuli to lumbar vertebrae for fMRI studies of chronic back pain
Radiation Analysis Dosimetry:A portable biodosimeter to measure radiation exposure using a blood sample
Simulation Innovation:Modifying a simulation experience in the OB/GYN Center
Wheelchair Seating Evaluation System: A device to assess the proper fit for people requiring a wheelchair
UR-PUCP Collaboration for Healthcare in Developing Nations: (This NCIIA-sponsored program provided opportunities for UR students to travel to Lima, Peru to address healthcare challenges in developing nations. In some cases, our students partnered with engineering students from Pontificica Universidad Catolica del Peru.)
DPN Diagnostics:Measurement of foot pressures to identify risk of ulceration in peripheral neuropathy, 2nd Place Forbes*
Medical Lighting: Inexpensive and effective illumination for dental and general examination
Peruvian Pulmonary Bed: A bed to facilitate postural drainage for treatment of pulmonary disease
( back to top)
Class of 2009
AFO—Ankle Foot Orthotic: Customizable ankle orthotic system
CDHSilo: Device to repair congenital diaphragmatic hernias
Independent Environmental Access (iCan): Hospital room control for patients with spinal cord injuries
MicroEZmix by Pocket Dose: Apparatus/procedure to aid in mixed dosing of injectable drugs, 2nd Place Forbes*
Nanomembrane Array for High-Throughput Drug Screening: Detection of proteins using a silicon membrane array
Operation Respiration: A neonatal respiration monitor for infants on high-frequency ventilation systems
PolyNet Technology: Evaluation of a shape-memory polymer as an intervertebral disc replacement, 1st Place Forbes*
TB-dx Microscopy Systems:Microscope adaptation for automated diagnosis of TB in developing nations
THERASSIST: Seating system for physical therapist using a treadmill to facilitate gait retraining
UltraNeedle: Apparatus to aid in the positioning of a needle during ultrasound procedures
Urine Oxidation: System to test for anti-oxidants in urine
Walk2: Device to improve muscle stimulation to prevent foot drop in patients with hemiparesis
( back to top)
Class of 2008
Salivary Protein Inspection Team (SPIT): A UV-visible spectrophotometer to monitor proteins in saliva, 1st Place Forbes*
Smart Toilet M.D.: Smart toilet to measure prescription compliance for prolonged independent living, 2nd Place Forbes*
Access-a-Pill: Device to dispense and cut medication for persons with accessibility issues
Vascular Engineering Group:Improvements to femoral artery stents for decreased fracture rate
Bridging the Gap:A method to measure the misfit of a dental implant
Bioelectric Solution Technologies: Bronchoscope induced electroporation for non-viral intrapleural gene transfer
Fracture Detective:Using ultrasound for the detection of bone breaks
Soft Tissue Viscoelasticity:Cyclic shear testing to characterize viscoelastic properties of soft tissues
Recovery on a Roll: Gait training with partial weight support
Building Balance:Assessing weight-bearing during recovery
Class of 2007
SOLUX Smile: Proprietary lighting system to help dentists match dental implant colors, 1st Place Forbes*
SLIDE Saline Solutions:Mechanically assisted syringe, Tie for 2nd Place Forbes*
INFUTECH Infusion Pump:Modifications for accessibility in home infusion pump systems, 1st Place RERC# Competition
URTEC-AS: wireless urine detector with alarm for toilet training system for children with autism
Rise-To-Relief Ramp: Customized ramp that aids a child with arthrogryposis to reach height of toilet
CAT-DS: An acoustic system that characterizes blood vessel obstructions using a sound profile
LumbarJacks:Device for treatment of lumbar spinal stenosis
VasculoVations: Flexible introducer sheath
( back to top)
Class of 2006
NanoNet: Design of Serial-Filtration System, 2nd Place Forbes*
Dynamic Diagnostics: Design of a Muscle Activity Monitor
Dex Innovations: An Accessible Medication Dispenser, 1st Place RERC# Competition
ACCEL: The portable head acceleration measuring device
TNGS: The Next Generation Stent: Improvement to the transjugular intrahepatic porosystemic shunt
Systolic Systemics: Design of a continuous non-invasive blood pressure monitor
PPC, Inc.: Practical Procedure Consultants: Design of a system to prevent lost guidewires
Pentocular: Non-invasively measuring the quality and quantity of tear film
Class of 2005
PAHLS: Personally adjustable hearing loss simulator, 1st Place Forbes
VersaErg Innovations: Accessible cyclic ergometer for diverse abilities, 3rd Place in Forbes* and 1st Place RERC# Competition
EM Need:Biopsy needle for reduced blood loss
AFB Robotics: Robotic needle and phantom for prostrate brachytherapy
Hydrogenyx Hydrodynamic Bioreactor:A multi-cartridge laminar flow
Whisker Wigglers:Rodent whisker stimulation device for experimental research
Globin, Inc: Bedside Blood Analysis
JREAM Co.: Physical activity & nutritional education for pediatric obesity
*Forbes Entrepreneurship Award: Honors the student or group of students judged to have submitted the best written and oral business proposal for their design
RERC-AMI Competition: NSF-sponsored National Student Design Competition to improve accessibility of medical instrumentation, judged by preparation of web page detailing design process and prototype
( back to top)
Online galleries of our projects on HAJIM's Design Day Website:
BME Student Project GalleryCMTI MS Student Project Gallery
( back to top)


